Start to Finish Veneers: Part 1, Treatment Planning
Many patients present to the dental office seeking cosmetic procedures to improve the appearance of their teeth and smile. Although teeth contribute to many biologic functions in humans, the importance of teeth as social devices should not be overlooked, as multiple studies relating dental esthetics to oral health related quality of life have correlated poor dental esthetics with psychosocial discomfort, and even poor dental hygiene in certain populations [i,ii]. With the advent of adhesive techniques and advanced dental materials, dentists have the opportunity to improve or enhance dental esthetics in a variety of patient populations using minimally invasive techniques and biomimetic principles. Through a three-part article, the requisite steps to provide responsible esthetic improvements will be covered in detail. This portion will focus on treatment planning and case design.
Figure 1; a) The 12 photographic views for AACD accreditation.
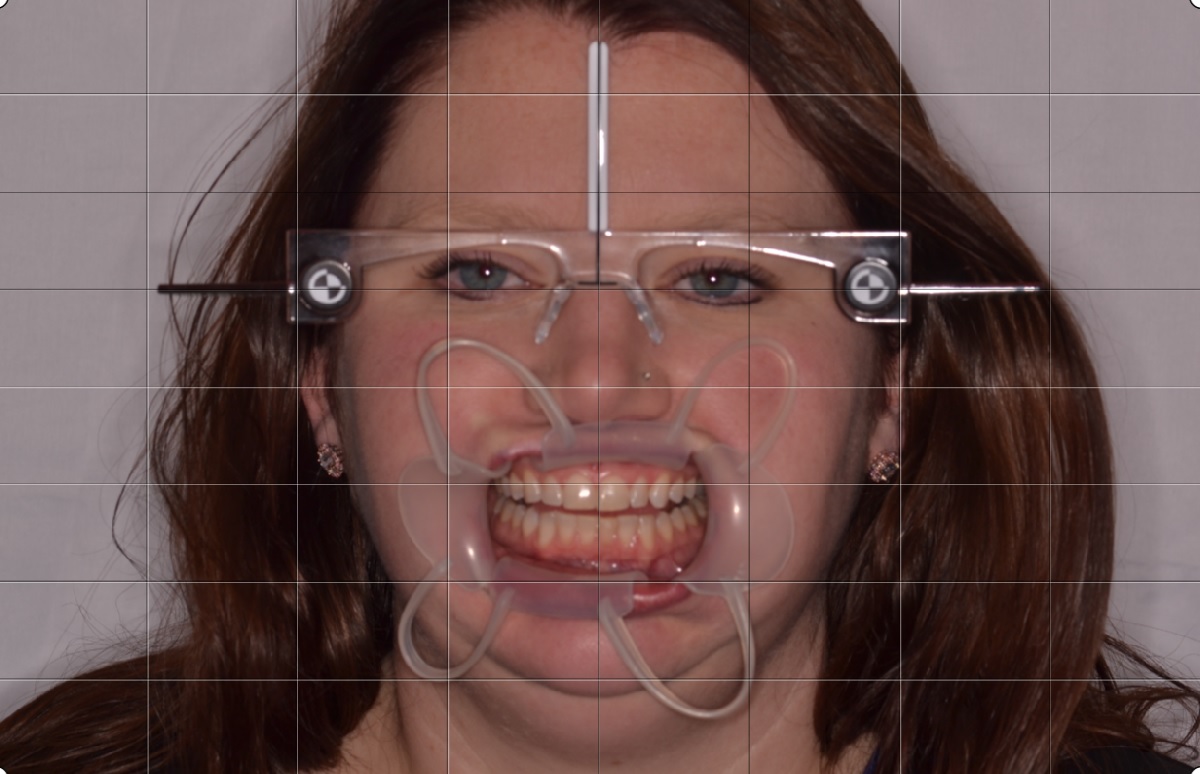
Figure 1b-d; b) Duchenne Smile (“E” smile) photo to evaluate lip mobility when muscle recruitment is high; c); Lip in repose photo to evaluate incisal edge position; d) Kois Facial Reference Glasses photo to evaluate maxillary plan and midline.
Figure 1; e) Shade tab photos for patient evaluation.
A 31-year old female presented to the dental office seeking improvements to her smile. The patient reported a history of orthodontic treatment, and expressed a desire to avoid orthodontic treatment if possible. Her chief complaint about the appearance of her teeth was the yellow color, despite repeated attempts to whiten with external bleaching. The patient also reported aversions to the incisal edge discrepancy, the overall length of her teeth, and the distally rotated upper left lateral incisor.
When planning large cases, the first step is to acquire and collate the necessary data. Photos were taken with a Digital Single Lens Reflex (DSLR) camera and macro lens before impressions were made. There are 16 photos the author considers essential. Twelve of the photos are the views required by the American Academy of Cosmetic Dentistry for accreditation [iii,iv] which consist of:
1. Natural Full Face – frontal angle – 1:10 (1:15) magnification
2. Full Natural Smile – frontal angle – 1:2 (1:3) magnification
3. Full Natural Smile – right lateral angle – 1:2 (1:3) magnification
4. Full Smile – left lateral view – 1:2 (1:3) magnification
5. Upper and lower teeth slightly parted – frontal view – 1:2 (1:3) magnification
6. Upper and lower teeth slightly parted – right lateral – 1:2 (1:3) magnification
7. Upper and lower teeth slightly parted – left lateral – 1:2 (1:3) magnification
8. Maxillary anterior in view only – frontal view – 1:1 (1:1.5) magnification
9. Maxillary anterior in view only – right lateral – 1:1 (1:1.5) magnification
10. Maxillary anterior in view only – left lateral – 1:1 (1:1.5) magnification
11. Maxillary arch – occlusal view – 1:2 (1:3) magnification
12. Mandibular arch – occlusal view – 1:2 (1:3) magnification
In addition, four adjunct photos are taken:
13. Duchenne Smile or Exaggerated (“E”) Smile photo (to evaluate lip mobility during a genuine smile)
14. Lip in repose (lip at rest) photo (to evaluate incisal edge position)
15. Kois Facial Reference Glasses with retraction (to identify any cants or midline discrepancies)
16. Shade tab photos (to assess patient preference for final shade)
(figure 1a-e)
The goal of the Duchenne Smile photo (“E” or Exaggerated Smile photo) is to activate the zygomatic major muscle and the orbicularis oculi muscle to provide perspective on tooth display that may only occur during a genuine smile (which is often difficult to replicate in the dental office). This photo is achieved by simply asking the patient to produce the biggest smile possible. Although there is variability in lip form, the lip in repose photo should focus on the canine, as Dr. Carl Misch concluded the canine exposure dimension relative to the upper lip in repose can be used to predictably assess anterior incisal edge position [v]. The patient is asked to say “Emma” and the photo is captured after the last syllable. The Kois Facial Reference Glasses are outfitted with horizontal and vertical reference planes and offer a chance to evaluate the current maxillary occlusal plane for cants that may need to be corrected, as well as the opportunity to correct midline cants or discrepancies. Shade tab photos are an excellent communication tool for the patient, laboratory, and dentist when determining the final shade in the definitive restorations. The shade tab should be aligned vertically and on the same plane as the teeth to be modified, and the shade tab label should be visible in the photo.
After photos are taken, high quality impressions are made (or full arch intra-oral scans are taken). The importance of taking impressions AFTER high quality photographs are taken should not be overlooked, as residual impression material can negatively affect otherwise excellent photographs. The impression technique used here utilizes a PVS heavy body putty and a PVS light body wash to capture as much detail as possible. Taking an inter-occlusal record can be challenging in some cases, and it is important to consider that certain patients may need to be treated to an orthopedically stable temporomandibular joint position, or Centric Relation Position, instead of an inter-cuspal position. If this is necessary, the most stable position of the joint should be determined and registered prior to restorative therapy. Fortunately, this patient had no signs of Temporomandibular Joint Dysfunction (despite evidence of occlusal interferences), and the inter-cuspal position was accepted as the treatment position.
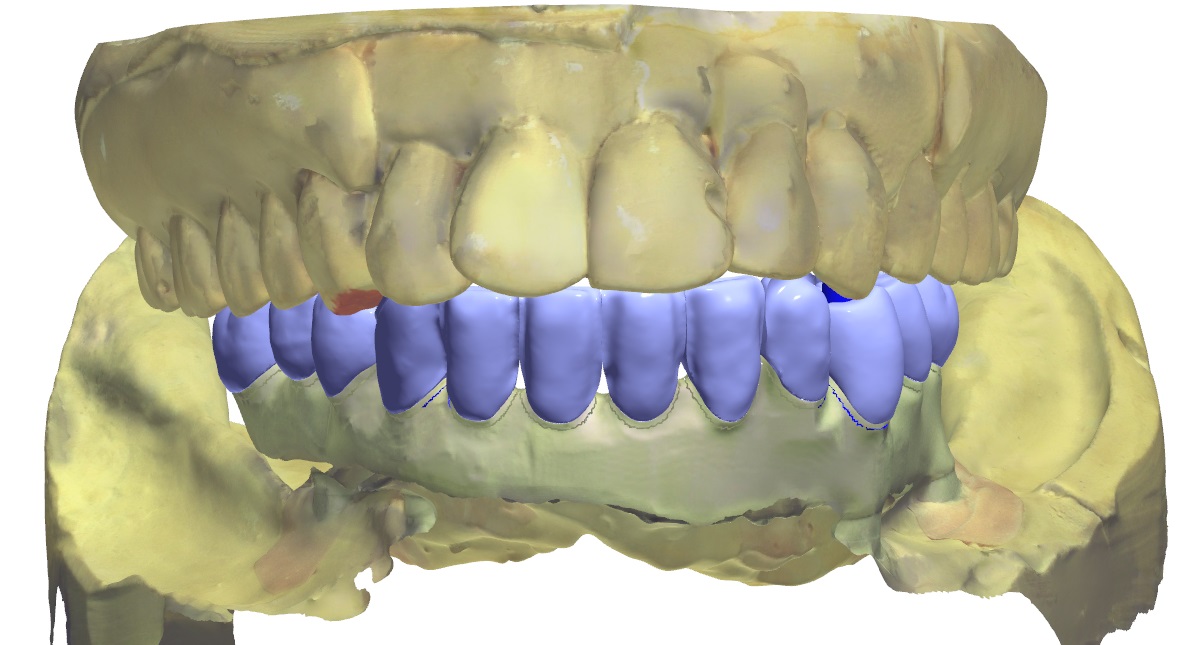
Figure 2; Evaluating gingival heights and contours.
Currently, Computer Aided Design and Computer Aided Manufacturing (CAD/CAM) technologies are utilized in the majority of the author’s case planning, and have almost entirely replaced analog diagnostic wax-ups. For this case, definitive casts were made from the PVS impressions and mounted on a semi-adjustable articulator (Panadent). The casts and mounting were scanned into 3Shape CAD/CAM software. From here, the digital design process could commence. Although the main indication for veneers in this case was a patient desire for whiter teeth that were resistant to external bleaching, the goals of this case design were also based on smile design and dental esthetic principles [vi]. The digital “wax-up” begins with the maxillary central incisors, as it is essential that these teeth are symmetrical. To achieve this, it is necessary to first evaluate gingival health, zenith heights, and contours, as the gingival shroud will frame the teeth and subsequently the smile. For this patient, it was determined that the gingival levels and contours were balanced and in an acceptable position to maximize smile design principles (figure 2)[vii,viii]; no gingival plastic surgery would be required. Next, the design focused on individual tooth proportion and relative tooth dimension. The pre-operative dimensions of the central incisors were 9 mm in height and 9 mm in width (a 100% width to height ratio), giving them a square appearance that lacked femininity. Having accepted the location and shape of the gingival tissues, length was added to the incisal edges of the maxillary central incisors so the new height would be 10.5 mm, while the 9 mm width was maintained (producing a more normative width to length ratio of 86%)[ix]. After the central incisors were designed, relative tooth dimensions and appropriate axial inclinations were applied to the lateral incisor and canine designs. Specifically, the malposition of the maxillary left lateral incisor was corrected in the CAD/CAM design, making light of an important part of the planning process: the data acquired from the plan will help dictate the eventual preparation design. In this way, conservative and minimally invasive preparations to achieve the final outcome can be executed relative to the initial design. This is a special consideration when instant orthodontics are to be performed using direct or indirect restorative materials, as areas where more or less tooth removal is required can be identified by overlaying the initial model scan and the idealized CAD/CAM design (figure 3a-b). Finally, the upper bicuspids on each side of the arch were included in the design to create harmony throughout the smile composition and control the patient’s buccal corridor. After completion, the digital design can be stitched to a digital photo to offer a prospective image approximating the appearance of the proposed restorative design in the patient’s smile (figure 4).
Figure 3a-b; The digital wax up overlayed on the pre-operative scan showing the difference in pre-operative tooth position and the proposed changes from a) an occlusal view and b) a frontal view.
Figure 4; A prospective image approximating the appearance of the proposed restorative design digitally integrated into the patient’s smile
The design is then manipulated in the digital space to evaluate the case from different perspectives. This allows fine tuning of intricate details related to tooth form such as facial line angle position, embrasure symmetry and balance, and even surface variation and texture [x]. Next, functional considerations are addressed. The patient’s static and functional occlusion is evaluated and refined using the digital articulator. For this case, canine rise was an achievable goal. Additionally, it was discovered that the patient had multiple occlusal contact on inclined planes and functional interferences when excursive movements were performed in the digital work-space on the programmed digital articulator (figure 5). This finding was confirmed clinically and it was determined that equilibration would be planned and performed prior to tooth preparation and the equilibration would be refined after delivery of the definitive indirect restorations.
Figure 5; Static and functional occlusal markings for each arch, clinically and digitally.
After the case design is finalized, a model of the desired case outcome is printed using a 3D printer. This model is important in fabricating deliverable items that are essential to not only a good case outcome, but to a minimally invasive preparation design that will encourage biomimetic restoration of the teeth. First, a facial reduction guide is made. When the teeth included in the treatment plan are prepared for veneers, this index provides the operator a reference to areas where more or less reduction of tooth structure is necessary as it relates to the thickness of the restorative material. For this case, the goal will be to produce thin lithium disilicate (IPS eMax, IvoclarVivadent) veneers that will range in facial thickness from 0.5 mm to 0.7 mm [xi]. When compared to the pre-operative condition, the facial reduction guide aids the clinician in planning removal of tooth structure in a way that is conservative and consistent with the desired outcome. Additionally, an incisal reduction guide is made to offer a preparation reference that will replicate the final incisal edge positions of the restorations and ensure the ceramic technician has space to create incisal characteristics such as translucency and microanatomy. For this case, the desired thickness of restorative material at the incisal edge is 1.5 mm. Lastly, a fairly rigid silicone index of the model is made from the printed model of the mock-up [xii]. Not only will this index be used to provisionalize the case with a working prototype, but the index can offer a preliminary evaluation of the case outcome and offer an adjunct method for determining the necessary amount of facial reduction (figure 6a-f). To transfer the mock-up, the index is loaded with an auto-cure temporary composite acrylic material (Visalys Temp, Kettenbach Dental) and overlayed onto the existing teeth with no preparation or adhesive. The material is allowed to cure before the index is removed and gross excess material is trimmed. At this time, the prototype is evaluated by the clinical and the patient. Important photographs are taken evaluate the proposed design and to ensure the midline is perpendicular and aligned with the face. Tooth shape, length, proportion, and axial inclination is also evaluated. Shade can be roughly estimated at this time, as many provisional materials come in esthetic shades. After the prototype design is validated by the operator and patient, the preparation phase of treatment can begin (figure 7a-d).
Figures 6a-f; a) A facial reduction guide made to the proposed result; b)The facial reduction guide compared to the pre-operative model; c) An incisal reduction guide made to the proposed result; d) View of the proposed changes to the current incisal edges; e) A silicone matrix to transfer the mock-up (pre-operatively and for provisionalization); f) Wedges cut into the gingival embrasure spaces of the matrix to provide a spillway for excess provisional material.
d
Figure 7a-d; a) Full Smile – left lateral view – (1:3) magnification; b) Natural Full Face – frontal angle – 1:10 (1:15) magnification; c) Kois Facial Reference Glasses photo with mock-up in place; d) Upper and lower teeth slightly parted – frontal view – 1:2 (1:3) magnification
Integrating appropriate patient data and communicating appropriately with a capable dental laboratory are paramount to achieving ultimate success in cases dealing with functionally esthetic corrections and smile design. Careful thought must be given to the design process and dentist must avoid a “prep and pray” modality of rendering treatment. Involving the patient in the process is recommended, as patient input offered in the planning stages of treatment can not only increase overall satisfaction with the outcome, but can save expense and time in the restorative stages of treatment. Moreover, thorough planning with all parties involved (dentist, technician, patient) can be very rewarding and make planning cases like this extremely fun!
Dr. Ryan J. Yakowicz, DDS, FAGD
Dr. Yakowicz practices in the Greater Madison Area of South Central Wisconsin. Having completed over 775 hours of continuing education, his special interests include functionally cosmetic full mouth rehabilitation, TMD and oral-facial pain, and surgical implant placement and prosthetic restoration.
Dr. Yakowicz is currently the president of the Madison Dental Progress Forum Study Club and the Wisconsin Institute for Advanced Dental Education. He is a Fellow of the Academy of General Dentistry, and a member of the American Academy of Cosmetic Dentistry, and the American Academy of Fixed Prosthodontics. Additionally, Dr. Yakowicz participates in research studies for the National Provider-Based Research Network and is an Ambassador to the National Health Service Corps.
References:
[i] Silvola AS, Varimo M, Tolvanen M, Rusanen J, Lahti S, Pirttiniemi P. Dental esthetics and quality of life in adults with severe malocclusion before and after treatment. Angle Orthod. 2014 Jul;84(4):594-9.
[ii] Solomon D, Katz R, Bush A, Farley V, McGerr T, Min H, Carbonella A, Kayne J. Psychosocial impact of dental esthetics on periodontal health, dental caries, and oral hygiene practices of young adults. General Dentistry. 2016 March/April; 64 (2): 44-50.
[iii] American Academy of Cosmetic Dentistry. “A guide to accreditation photography: Photographic documentation and evaluation in cosmetic dentistry.” Madison, WI: 2009-2015.
[iv] Terry DA, Geller W. Esthetic & restorative dentistry: material selection & technique. Chicago: Quintessence Pub. Co., 2013: 553-572.
[v] Misch CE. Guidelines for maxillary incisal edge position-a pilot study: the key is the canine. J Prosthodont. 2008 Feb; 17(2): 130-134.
[vi] Magne P, Magne M, Besler, U. Natural and restorative oral esthetics. Part 1: Rationale and basic strategies for successful esthetic rehabilitations. Journal of Esthetic Dentistry 1993; 5: 161-173.
[vii] Rufenacht CR. Fundamentals of Esthetics. Berlin: Quintessence, 1990: 67 - 134.
[viii] Goodacre CJ. Gingival esthetics. Journal of Prosthetic Dentistry 1990; 64: 1-12.
[ix] Sterrett JD, Oliver T, Robinson F, Fortson W, Knaak B, Russell CM. Width / length ratios of normal clinical crowns of the maxillary anterior dentition in man. Journal of Clinical Periodontology 1999; 26:153-157.
[x] American Academy of Cosmetic Dentistry. “A guide to accreditation criteria: Contemporary concepts in smile design.” Maidson, WI: 2014.
[xi] “IPS eMax: Clinical guide.” Ivoclar Vivadent. (file:///C:/Users/ryany/Downloads/IPS+e-max+Clinical+Guide%20(1).pdf)
[xii] Magne P, Besler U. Bonded Porcelain Restorations in the Anterior Dentition: A Biomimetic Approach. Chicago, IL: Quintessence, 2003: 239-246.
All-on-X Overview
The idea of providing an All-on-X implant supported prosthesis to a patient can seem overwhelming and complicated. Which of course, it is. All-on-X treatment is at least a full arch rehabilitation, and almost always includes extra considerations relating to surgical technique and treatment sequencing. In this way, the dentist interested in restoring an edentulous arch with a full arch, implant supported dental prosthesis is encouraged to attain not only specific training in All-on-X techniques, but have advanced knowledge of gnathology, occlusion, and the functionally cosmetic demands of conventional denture design. The idea of referring a patient to an oral surgeon for four implants and taking a in impression of the implant position to send to a laboratory to fabricate a full arch prosthesis is insufficient in plan and execution, and will most likely yield poor results for the patient and expensive mistakes for the doctor.
A strong and compelling argument can be made that the first step of providing successful All-on-X treatment is denture fabrication, especially in the case of a totally edentulous patient. Prosthodontic principles such as vertical dimension of occlusion, incisal edge position, tooth size and shape, and phonetic considerations must all be determined prior to definitive restorative therapy. Perhaps the best way to ensure a functional and cosmetic implant supported denture that allows the stomatognathic system to function optimally is to first create a conventional denture that looks good, feels good, and chews good (well), without creating occlusal-muscle problems or speech difficulties. A full arch conventional denture can be used as an interim restoration that fulfills functional and social needs during the healing phase after implant surgery.
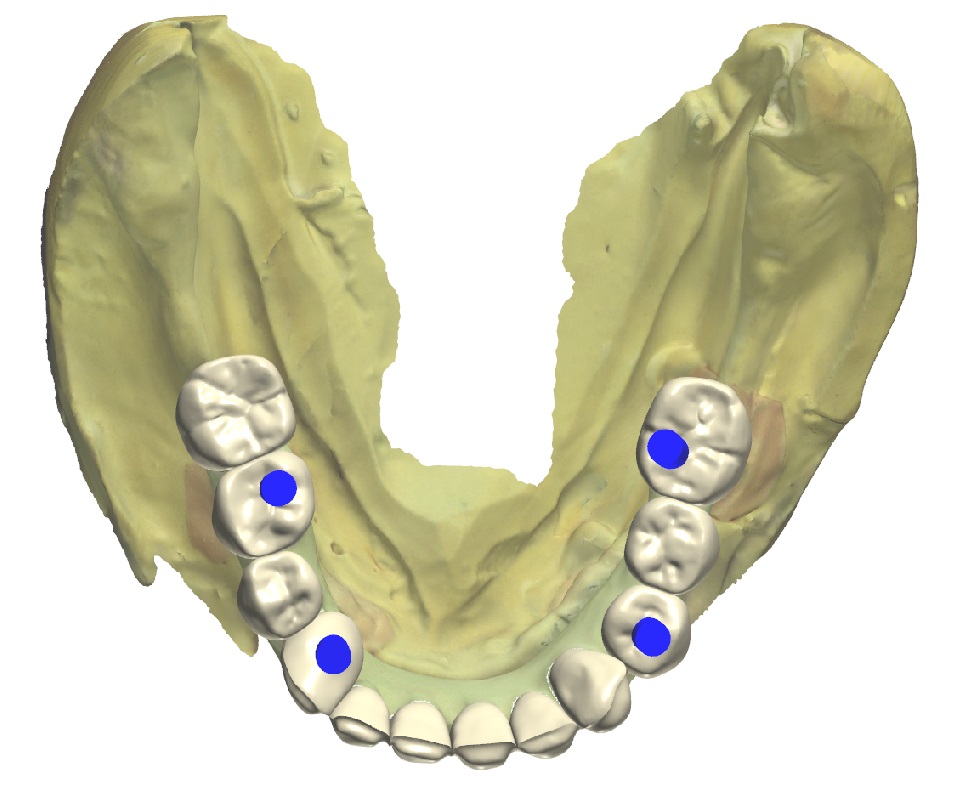
Figure 1a; The edentulous mandible.
Figure 1b; A conventional mandibular denture
Once the provider has established an appropriate VDO and functionally cosmetic tooth position, implant placement relative to vital structures and bone volume and quality can be considered (figure 2). Ideally, implant placement should pay some credence to the final design of the restoration. Currently, integrating digitized models or intra-oral scans with Cone Beam Computed Tomography can provide accurate treatment planning and surgical guidance for such a procedure. If the patient has abundant quantities of dense bone is present, the surgical placement of dental implants may be done free hand, and may even utilize angulation guides from dental implant manufacturers to assist in implant placement. Of course, a surgical drilling guide can be utilized as well, and in either case, there are distinct advantages to evaluating a patient three dimensionally with integrated Standard Tesselation Language (STL) renderings of teeth stitched to a CBCT versus historical methods of 2D panoramic films and stone models. If the surgery is to be carried out with the use of a guide, rigid fixation of the drilling appliance is essential. If the patient is fully or partially dentate at the time of surgery, teeth without severe periodontal disease or mobility can provide hard tissue support for the guide (figure 3a, 3b). If the patient is edentulous, fixation screws can aide in holding the guide in a fixed position and ensure accurate execution of the surgical plan. After implant placement, an experienced provider may immediately temporize the patient with an interim fixed denture in the form of a new prosthesis or a converted existing denture, given good primary stability of each implant. In other cases, healing abutments may be placed and the existing interim denture adjusted to accommodate them. The implants may also simply receive cover screws and be covered with soft tissue to allow healing or stage financing further treatment while wearing a functional interim conventional denture.
Figure 2; Digitally assisted planning of the implant position.
Figure 3a; Surgical guide consistent with serial extractions and maintenance of selected teeth for rigid support to accommodate proposed implant position.
Figure 3b; Pre-operative and post-operative panoramic radiographs.
After healing, the implants can be restored with a full arch prosthesis. There are many ways to achieve this. Locators or friction fit abutments may be utilized to retain a denture that is essentially “fixed” but can be removed by the patient for hygiene purposes. A bar may be utilized, or the prosthesis may be screwed directly to abutments already torqued to the fixtures. Inter-occlusal space is an important consideration here, as different prosthetic designs require different amounts of space to accommodate necessary components; 15 mm from the implant platform to the opposing occlusal surface is a good benchmark number to consider here. Ostensibly, even the task of being able to appropriately identify and name the components required for completing such an intricate dental prosthesis is itself challenging. Commonly, something called a Multi-Unit Abutment (MUA), or Multi-Base Abutment (MBA) is utilized as an abutment to link the fixture to the prosthesis. The MUAs are commonly inserted to a definitive torque of 25 - 35 Ncm (Figure 4). MUAs can be be offset to accommodate implants that were placed at an angle to avoid the mental foramen or maxillary sinus. Once the MUAs are in place, they stay put (barring implant complications). The MUAs have their own internal housing that will receive a screw to retain the prosthesis, which is torqued at a slightly lower value than the MUAs, commonly 15 Ncm.
Figure 4; Four multi-base abutments inserted to the fixture to a torque value of 25 Ncm.
Once the MUAs are placed, an abutment level impression is made to pick-up the implants’ spatial location and orientation relative to the arch. An impression post is screwed into each MUA, and the impression is taken with an open tray (figure 5). Many methods to ensure an accurate transfer of this information exist. In the pictured case, a 3D printed custom tray with rigid chimneys was used to provide stability of the impression posts in the impression, thereby ensuring accurate transfer of the implants’ location. Commonly, the impression posts may be joined with rigid fixation by way of pattern-resin covered floss or rigid wire that is luted to each of the impression posts. In any case, the next step is to have a master cast made with implant analogs in the stone cast. At this point, a verification jig is made on the master cast using replica cylinders. Clinically, the verification jig is inserted into the patient’s mouth and evaluated for accuracy and passive fit. It is essential that passive fit is attained, as a prosthesis that does not fit passively can contribute to bio-mechanical complications. To verify passive fit, the jig should seat evenly across all MUAs. Furthermore, the single screw technique should be utilized, whereby a screw is tightened into each MUA without any portion of the verification jig lifting out of place. Additionally, radiographs can be made to evaluate the intimacy of fit between the components. If the jig does not fit evenly or passively, do not panic. The jig can be sectional and re-luted with pattern resin to produce a now accurate jig (note the complete set time of the pattern resin here, as shrinkage of the resin can occur if the jig is removed prematurely)(figure 6). If the verification jig is altered intra-orally, the master cast is altered by the lab accordingly, as the implant analog location will have been found to be different from the initial impression and cast (figure 7). In this case, a wax rim was made to fit over the verification jig. This wax rim was based on the initial articulation of study casts using a duplicate denture as a guide for the final VDO. The wax rim can be altered to the desired VDO chair-side before an inter-occlusal record is made (figure 8).
Figure 5; Custom tray, and Multi-Base Abutment impression posts in place.
Figure 6; Laboratory fabricated verification jig and luting of the sectioned jig intra-orally to ensure passive fit of the framework.
Figure 7; Definitive altered cast with verification jig and wax bite rim at the patient’s current Vertical Dimension of Occlusion (VDO).
Figure 8; A duplicated denture was utilized in approximating the desired VDO of the definitive casts. The wax bite rim was built to the current VDO and an inter-occlusal record was made intra-orally after the wax bite rim position was adjusted and verified.
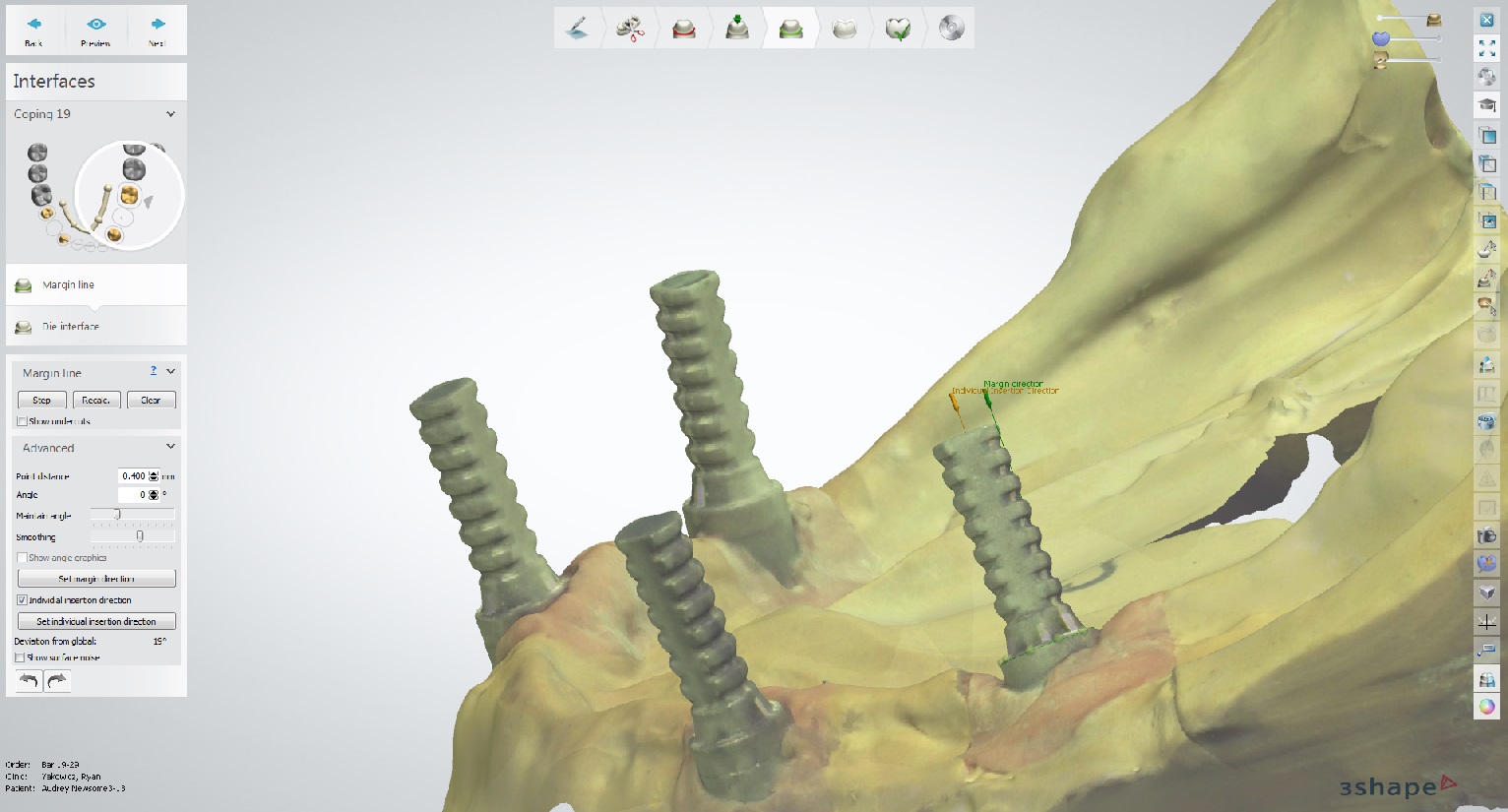
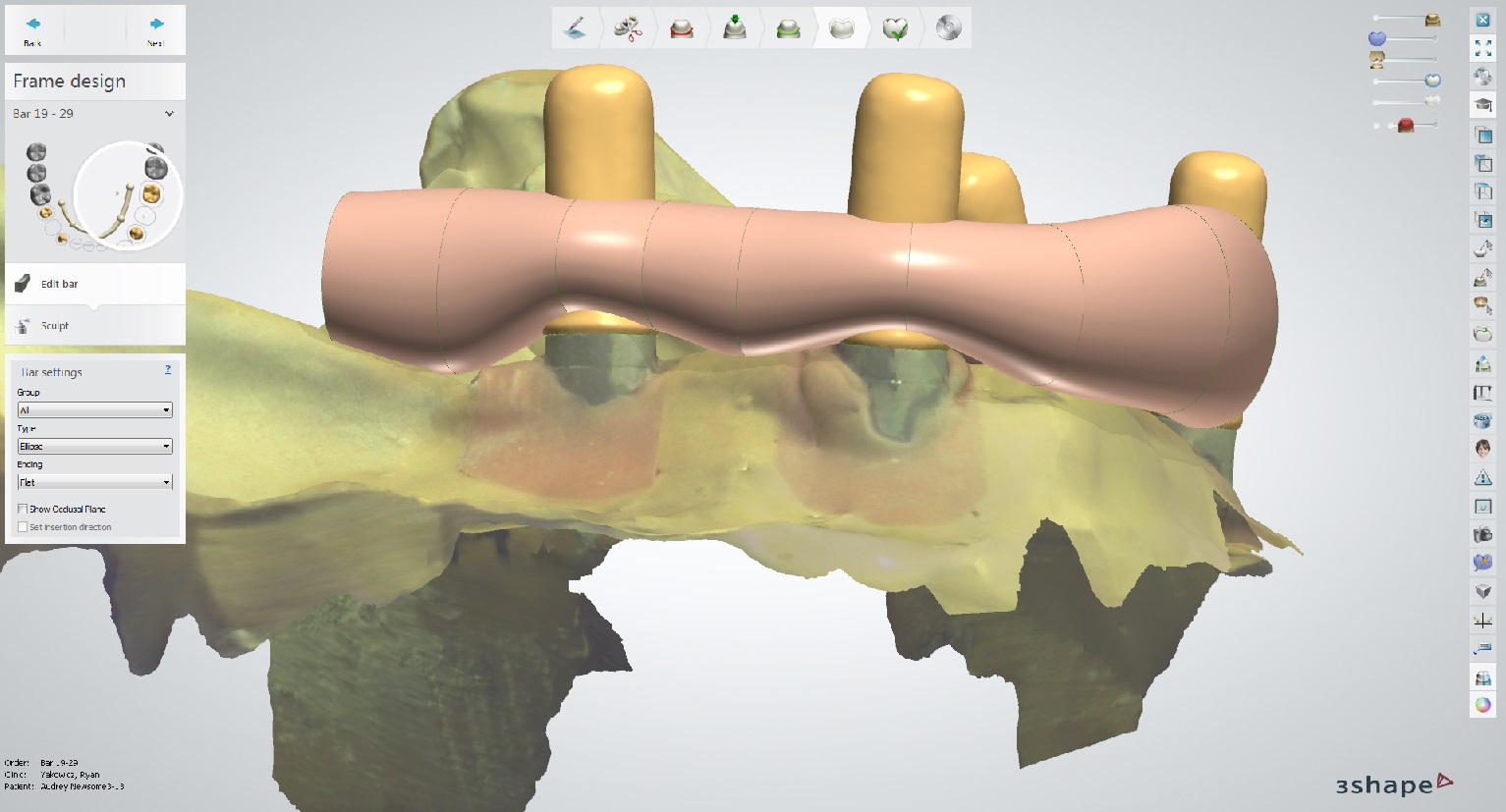
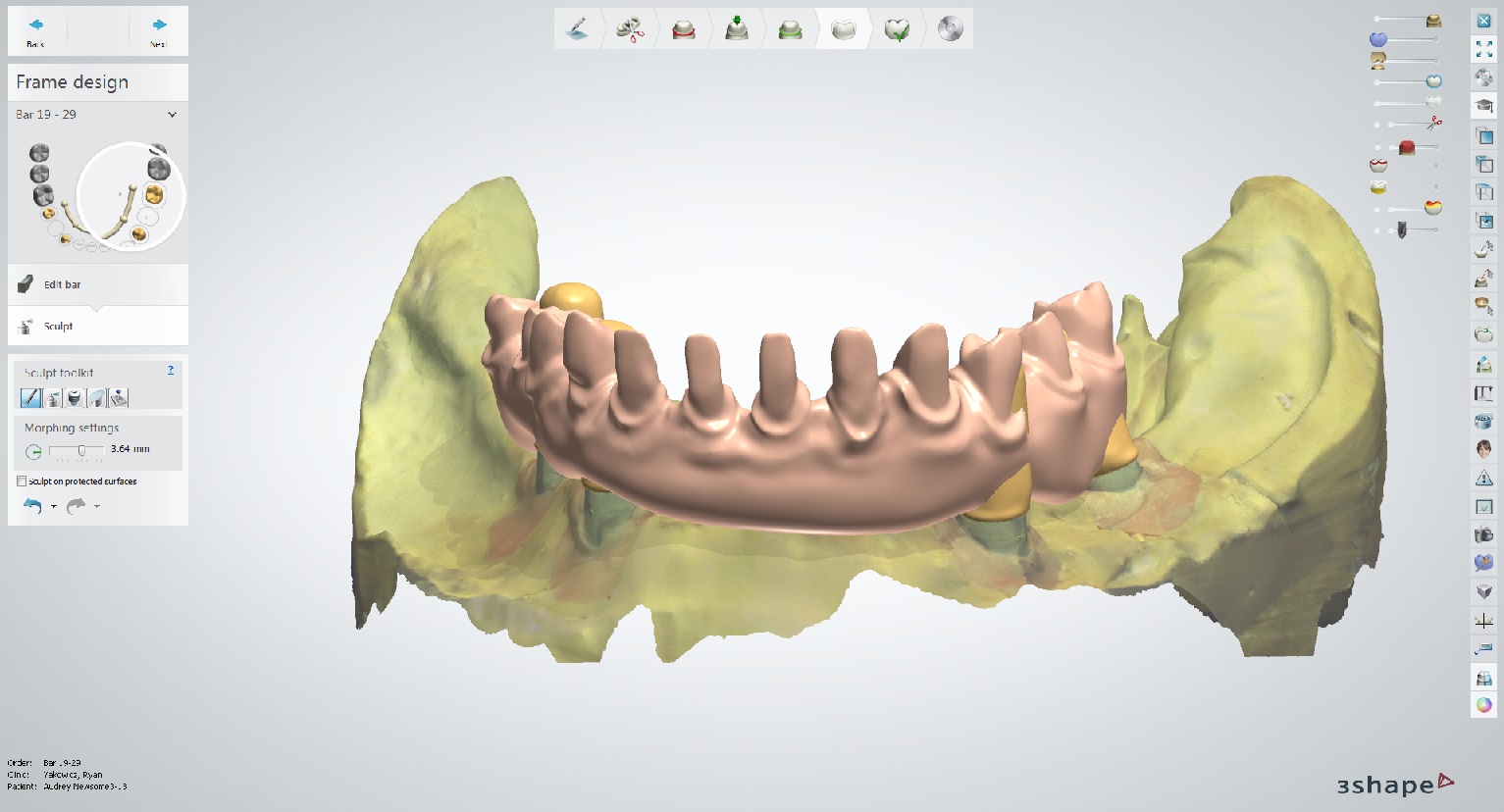
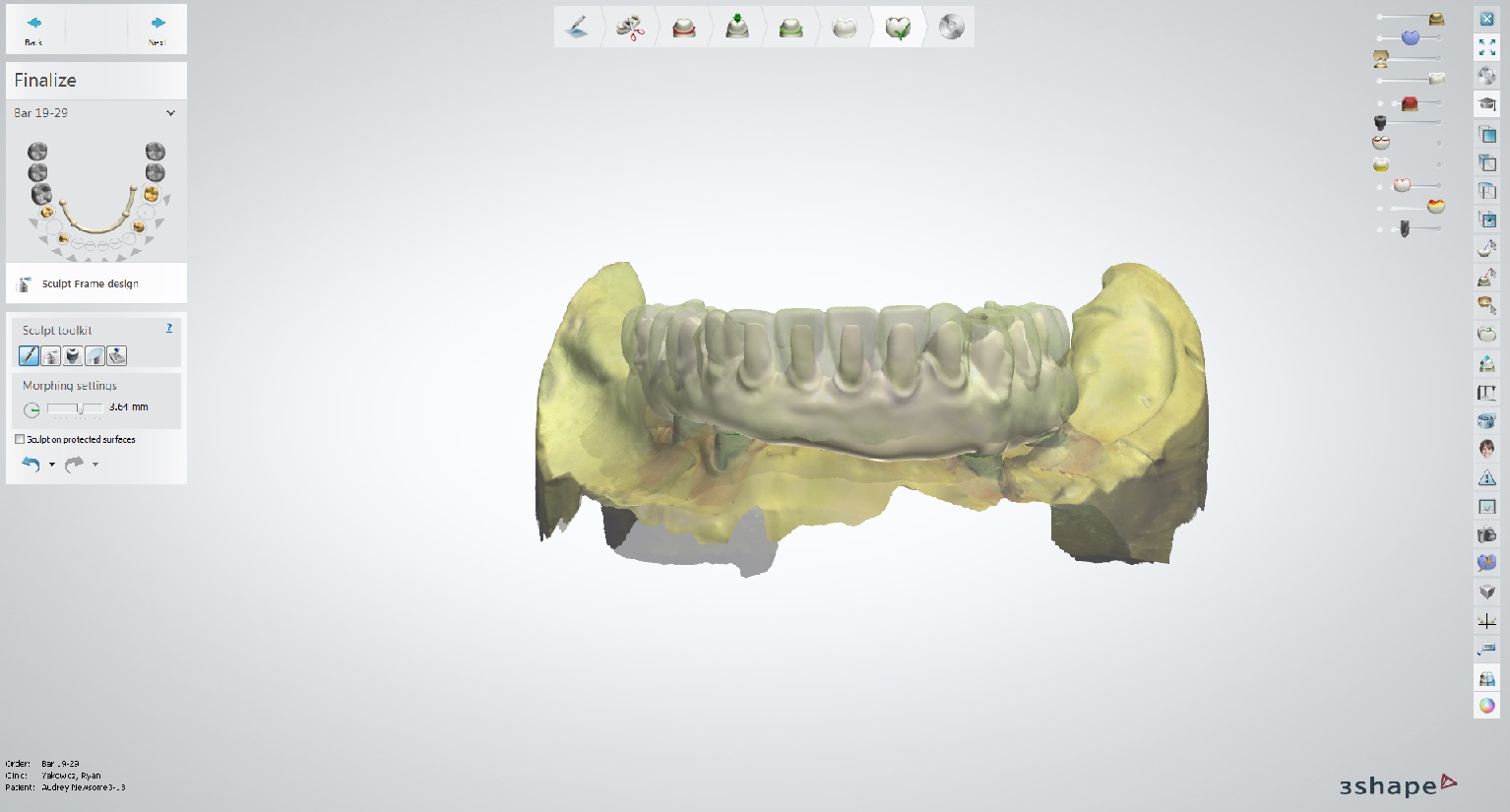
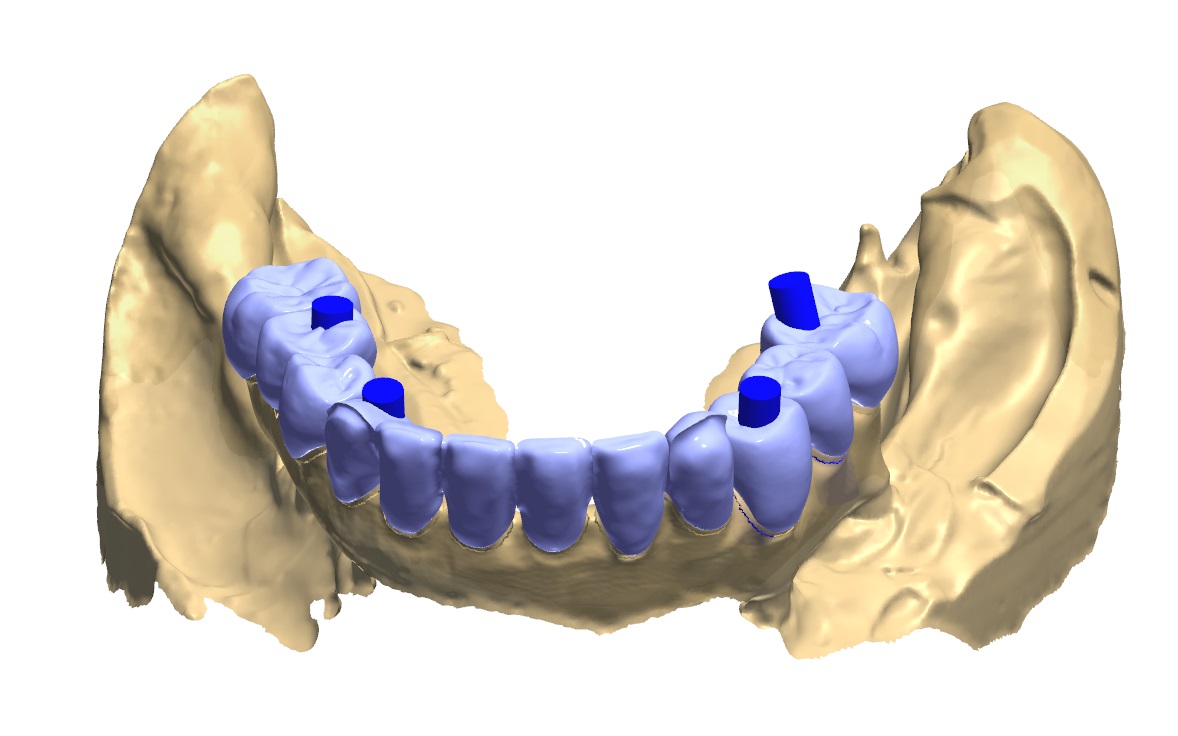
For this case, digital modalities were utilized to help create the final prosthesis. The existing model work was digitized, and a “crown down” digital design was created (figure 9a). Based on the overall occlusal scheme and tooth position, a framework was designed to accommodate individual eMax crowns on a PEEK (polyetheretherketone) framework hand layered with composite. A trial framework was milled out of PMMA to ensure fit to model, and, once verified, the framework was milled out of a PEEK puck, and cylinders to accommodate the intra-oral multi-base abutments were luted in place within the framework (figure 9b). Individual crown preps were milled into the framework design and the framework was re-scanned to design CAD/CAM crowns to the framework (figure 10). An adhesive bonding protocol exists for PEEK materials. As such, once the framework is roughened with a diamond bur, sandblasted with AlO2, and primed, an adhesive interface ensures solidarity of the components. After the eMax crowns are fired and glazed, they are conditioned before being bonded to the PEEK framework. Etching the intaglio surface of the crowns with 5% HF acid for 20 seconds followed by rinsing and drying and applying silane is done before the crowns are loaded with an adhesive resin cement and placed definitively onto the framework. The rest of the PEEK framework is hand layered in pink composite and cured, per manufacturer instructions. A glycerin barrier is applied before final curing to prevent the formation of an oxygen inhibited layer during the curing process, and the total prosthesis is highly polished (figure 11).
Figure 9a and 9b; Digital design of the prosthesis and the PMMA trial framework on the left and the definitive PEEK framework on the right.
Figure 10; Blue-phase individual eMax crowns fitted to the PEEK framework. The anterior is cutback for layering to amplify esthetics.
Figure 11; The fully processed definitive prosthesis (PEEK, eMax, Composite), ready for delivery.
Insertion protocol is relatively straightforward, given that the accuracy and passive fit of the prosthesis has been maintained during fabrication. The prosthesis fit is verified, and the occlusion is refined as necessary. The occlusal design has some set parameters, and some parameters that are dependent on the opposing arch.
Important things to always build into the design are:
Bilaterally identical occlusal contacts in the posterior and canines
Very slight to no contact on incisors
Freedom of movement through excursive movements (also referred to as “Freedom in Centric”)
No interferences on inclined planes (avoid any “tilting” forces)
Criteria for functional occlusion specific to opposing dentition include:
If opposing natural dentition/canines: Canine guidance.
If opposing implant supported frameworks: Group function with relatively flat cusps (less than the steepness of the condylar path, ascertained by the angle of the protrusive bite record) and limited vertical overlap.
If the implant supported prosthesis is opposed to removable partial denture, complete denture or implant supported over denture: Group function with a balancing contact to stabilize the removable prosthesis during function
The prosthesis is screwed into place with small bridge screws torqued to 15 Ncm each. An important part of the planning process for the prosthesis is location of the screw holes (figure 12). In this case, each screw hole was located on a lingual or occlusal surface of the prosthetic teeth. This is desirable in comparison to screw-holes that exit the body of the framework (gingiva) or in an esthetic area (facial or buccal surfaces of teeth). Once the screws are torqued into the multi-base abutments, polytetrafluoroethylene (PTFE) tape is placed over the screw access and covered with dentin shade or more opaque composite before a composite akin to the tooth shade is placed in an effort to combat a low value appearance of the screw access fill. The occlusion is adjusted as necessary and the composite restorations are polished.
Figure 12, Location of the screw access holes and access fill with composite, shown with initial occlusal markings.
Maintenance is an important and often overlooked part of this treatment. First, the prosthetic device should be designed with proper emergence profile and convex contours that enable spillways for debris. Second, patient hygiene practices are paramount. The patient is given a Waterpik and is asked to use it on a low setting (e.g. 3) to further facilitate debris removal from under the framework. The patient is asked to avoid the abutments with the Waterpik in an effort to protect the hemi-desmosomal connection to the multi-unit abutments. Instead, the patient is asked to use a Nimbus extra-soft bristled toothbrush to clean around the abutments. The recommended toothpaste is any low abrasive toothpaste in an effort to preserve the polish and luster of the restoration. The patient is also given Superlfoss for use under the bridge, and advised to use mouth rinse as he or she is willing or able. Lastly, the patient is scheduled for 1-year re-care visits (this timeline may be more or less frequent depending on patient risk factors or patient hygiene practices and how they relate to dutiful implant maintenance). The implants and associated tissues should be clinically evaluated and radiographs should be made at appropriate intervals. The Multi-Base Abutments should be cleansed of calculus or plaque using the correct instrumentation. Lastly, it is important to note that it is the position of the American College of Prosthodontists that removal of the prosthesis is not necessary unless there are “signs of peri-implantitis, a demonstrated inability to maintain adequate oral hygiene, or there are mechanical complications that require removal.”
As is evident by this journal entry, All-on-X treatment is complicated, and includes many treatment considerations. Esthetics, occlusion, biomechanics, surgical implant protocols, denture design, maintenance, and phonation all require attention and expertise if All-on-X treatment is to be performed. These types of prostheses can be very challenging, and require a lot of knowledge to execute properly. Ultimately, a well-made, full arch, implant supported prosthesis offers a high degree of satisfaction to provider and patient (figure 13a, 13b).
Figure 13a; Panoramic radiograph of the definitive prosthesis in place.
Figure 13b; A pre-operative (left) and post-operative view (right).
Dr. Ryan Yakowicz, DDS, FAGD
Dr. Yakowicz practices in the Greater Madison Area of South Central Wisconsin. Having completed over 775 hours of continuing education, his special interests include functionally cosmetic full mouth rehabilitation, TMD and oral-facial pain, and surgical implant placement and prosthetic restoration.
Dr. Yakowicz is currently the president of the Madison Dental Progress Forum Study Club and the Wisconsin Institute for Advanced Dental Education. He is a Fellow of the Academy of General Dentistry, and is a member of the American Academy of Cosmetic Dentistry, and the American Academy of Fixed Prosthodontics. Additionally, Dr. Yakowicz participates in research studies for the National Provider-Based Research Network and is an Ambassador to the National Health Service Corps
REFERENCES:
i) ACP Position Paper on the Maintenance of Full Arch Implant Restorations.
(https://www.prosthodontics.org/assets/1/7/Maintenance_of_Full-Arch_Implant_Restorations.pdf)
ii) Prosthodontic Perspective to All-On-4® Concept for Dental Implants
M Taruna,1 B Chittaranjan,2 N Sudheer,3 Suchita Tella,4 and Md. Abusaad5
J Clin Diagn Res. 2014 Oct; 8(10): ZE16–ZE19.
iii) Periodontol 2000. 2016 Jun;71(1):164-84. doi: 10.1111/prd.12122.
Post-treatment supportive care for the natural dentition and dental implants.
iv) Bonded Porcelain Restorations in the Anterior Dentition: A Biomimetic Approach (2003)
Quintessence Publishing Co, Chicago, IL
Magne, Pascal. Besler, Urs.
v) Dental Implant Prosthetics 2nd Edition. Elsevier Mosby, St. Louis, MO. Misch, C.
Soft Tissue Management and Laboratory Communication in the Esthetic Zone
Introduction
Early in my career I developed an interest in cosmetic dentistry and digital photography. As I completed and documented more cases, I noticed common issues arising when communicating with the laboratory and delivering final restorations. I frequently struggled to get the laboratory to make the interproximal contacts long enough to adequately close black triangles, and I would try in restorations and see exposed facial margins after temporization, and I lacked confidence when deciding if the tissue would rebound to an acceptable position (figure 1).
Figure 1; A black triangle upon delivery of veneers.
I found that when cases achieved the desirable outcome it was due to luck, and when the outcome was less than desirable it created considerable stress. Individuals have attempted to solve this issue, for example, Willi Geller developed a method referred to as the “Carrot Model” or “Geller Model” in which the individual dies are trimmed and inserted into a model replicating the soft tissue (figure 2a, 2b). [i] The downside to this option is this technique is quite labor intensive for the dental laboratory. At times, technicians have attempted to replicate soft tissue with silicone. The problem with this is often times they replicated tissue that was distorted after retraction.
Figure 2a; Geller model with dies in place
FIgure 2b; In the fabricated Geller master cast, the dies are removed coronally and the soft tissue in the casting is preserved.
Additionally, I would rely on statistical averages and share those approximate values with the laboratory, hoping that would be enough to achieve the ideal result. Despite all the efforts, the results were not as consistent as I had hoped. More recently, I have implemented a protocol to deliver results like that shown in figure 3 predictably.
Figure 3; Before and after closing a diastema with porcelain.
Figure 4; The desired outcome after indirect restorations.
So how does one go from treatment goal to desired final outcome predictably?
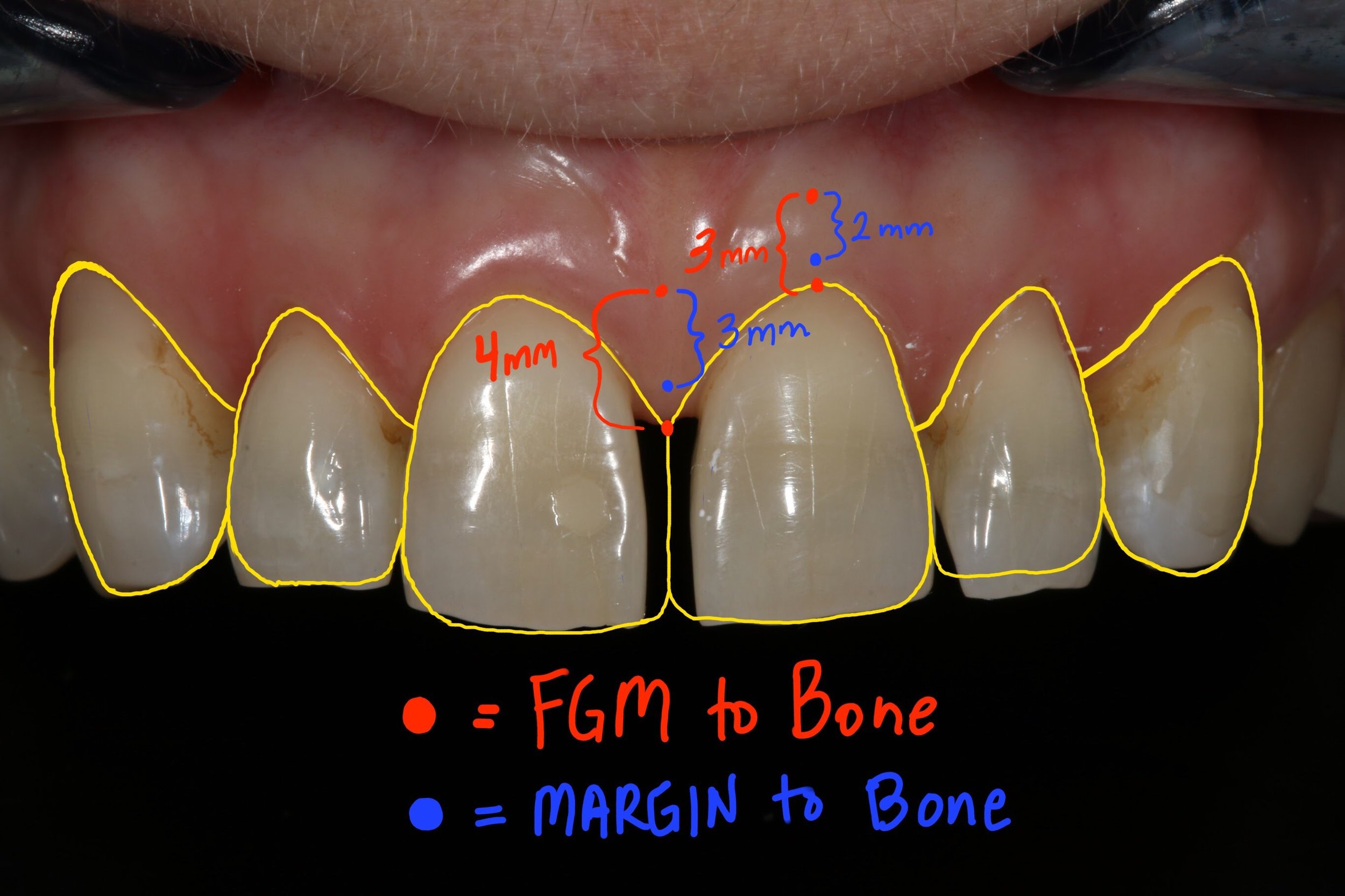
In 1961 Gargiulo et al. published research indicating an average biologic width of 2.04 mm, and a sulcus depth of .69 mm [ii]. However, due to human variability, and variation in probings per clinician, we must look at the dentogingival complex as a whole in order to achieve the desired cosmetic result (figure 4). A study of 100 healthy patients found an average distance from facial bone to gingival margin of 3 mm. [iii] Van Der Velden found an average interproximal distance from bone to papilla of 4.3 mm. [iv] The foundation for predictable soft tissue management begins with accurate assessment of these numbers both facially and interproximally at or before preparation. [iii] The following steps should be taken when preparing teeth to be restored in the esthetic zone:
1. Administer local anesthetic.
2. Sound the bone level through the gingival attachment to the osseous crest (with periodontal probe at ~ 45 degree angle).
3. The gingival margin should be 3 mm from bone on the facial and 4 mm from bone interproximally in those patients with a normal crest relationship (figure 5).
4. Prepare the tooth without retraction, margin location should be 2 mm from bone on facial, and 3 mm from bone interproximally. This ensures the margin will not be visible, while not invading the biologic width (figure 5).
5. Instruct the laboratory to make the most apical interproximal contact point 1 mm from margin. This will ensure papilla rebound to fill the black triangle (figure 6).
Figure 5; Gingival and crown margin distance to bone
Figure 6; Distance from gingival margin to preparation margin
Figure 7a; Black triangle closure using the proposed protocol and laboratory instruction for predictable soft tissue results (1:1 magnification view)(Case and photos by Dr. Ryan Yakowicz)
Figure 7b; Black triangle closure using the proposed protocol and laboratory instruction for predictable soft tissue results (3:1 magnification lateral view)(Case and photos by Dr. Ryan Yakowicz)
If we have done our due diligence at or prior to preparation, we know the gingival margin and preparation location in relation to the bone. Despite distortion at the time of insertion, we can say with confidence whether these restorations will achieve harmony and proper esthetics with the tissue as it matures, even if a black triangle or visible margin exists initially upon delivery of the final restorations (figure 7a, 7b).
Dr. Austin Wessell, DDS
Dr. Wessell maintains a private general and cosmetic dental practice on the far west side of Madison, Wisconsin. Having completed hundreds of hours of continuing education, his interests include cosmetic and full mouth rehabilitation, cosmetic bonding, surgical implant placement, and dental photography.
Dr. Wessell is currently a member of the Madison Dental Progress Forum, the Academy of General Dentistry, the American Academy of Cosmetic Dentistry, and the Chicago Dental Society. Additionally, Dr. Wessell participates in Spear Study Club and is an avid student at the prestigious Kois Center in Seattle, Washington.
[i] “The Carrot Model”
Tric O
Spectrum Dialogue, Vol. 9 No. 2, February 2010
[ii] Dimensions and relations of the dentogingival junction in humans.
Gargiulo AW, Wentz FM, Orban B.
J. Periodontol 1961; 32: 261-267
[iii] Altering Gingival Levels: The Restoration Connection Part 1: Biologic Variables
John C. Kois DMD, MSD
Journal of Esthetic Dentistry
Vol. 6, Number 1 1994
[iv] Regeneration of the Interdental Soft Tissues Following Denudation Procedures
van der Velden U.
J Clin Periodontol. 1982 Nov;9(6): 455