Start to Finish Veneers: Part 3, Insertion with Adhesive Bonding
As evidenced by the previous two posts in this sequence, planning and preparing teeth for functionally cosmetic restorations is a demanding process that requires diligence, time, and expertise. The provider and patient should both be extremely excited for the final result of the hard work and time that has been invested. Although communication with the laboratory and the skill of the ceramist are critical factors in determining the final outcome, only after careful case planning, meticulous tooth preparation, and successful prototyping of the project, can successful delivery of final ceramics can be considered.
Figure 1; Presentation of patient and provisionals at delivery appointment
The importance of home-care and dental hygiene instructions for the duration of the provisional use is paramount, as an isolated field free of heme and debris is supremely advantageous for inserting cosmetic ceramic restorations with an adhesive bonding technique. Fortunately, the patient in this case was able to maintain good oral hygiene and presented with healthy gingiva that showed little to no sign of inflammation (figure 1). In cases where gingival inflammation will create heme that will interfere with adhesive bonding techniques, placing retraction cord in the gingival sulcus must be considered.
Before removal of the provisional restorations, the patient is anesthetized. This can be done with conventional buccal and facial infiltration techniques, or from the palate in an effort to preserve lip mobility in order to evaluate the smile and presentation of teeth relative to upper lip dynamics.
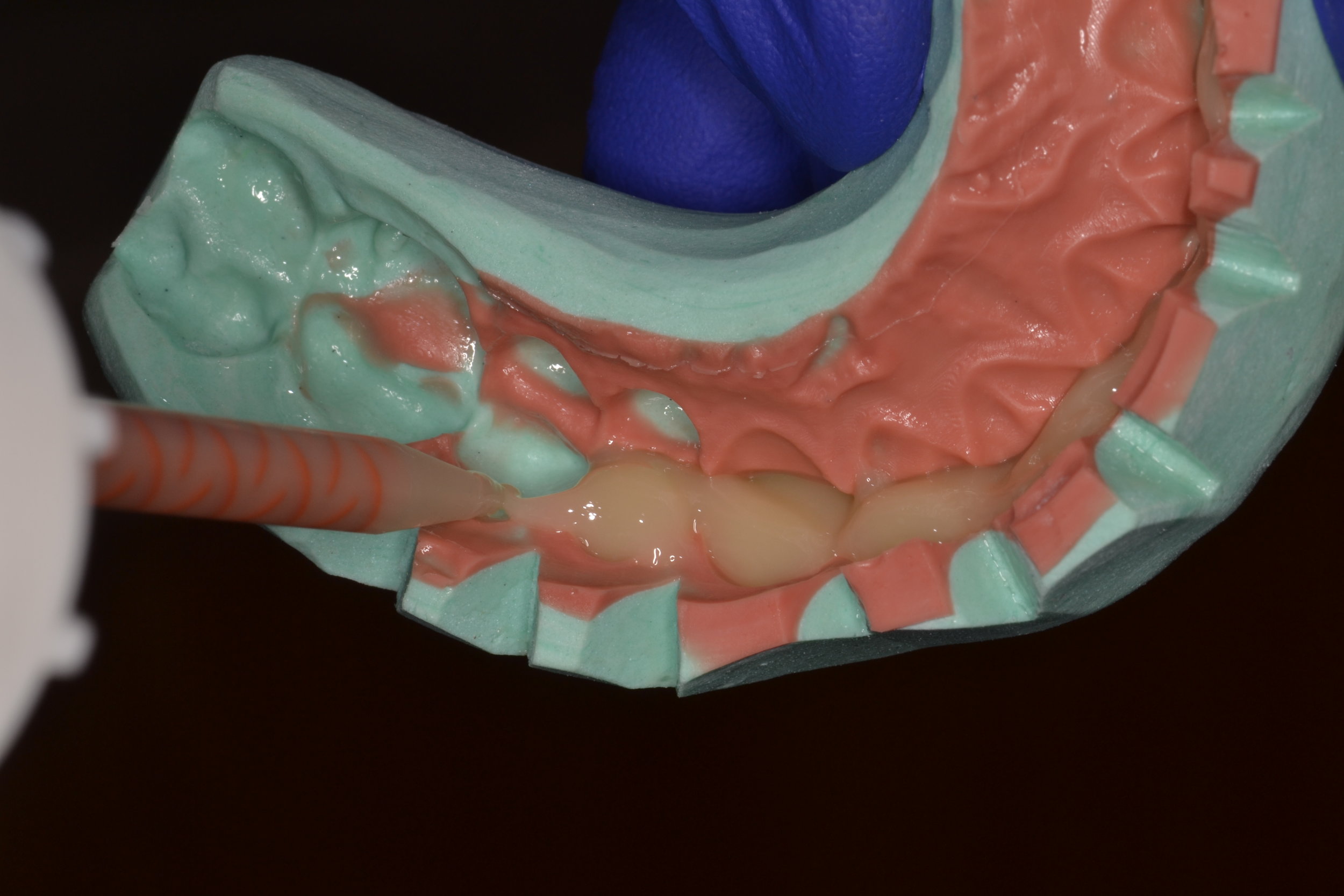
After the patient is comfortably numb, the provisional restorations are removed. Since a shrink-wrapping technique was used in this case, the provisional restorations are connected. A hemostat is used to crush and fracture the acrylic material in interproximal areas (figure 2). After gross removal of the temporary restorative material, hand instruments like scalers can be used to facilitate complete removal (figure 3a). The preparations are then polished using an oil-free flour of pumice (figure 3c), as the oil content in regular polishing paste commonly used for dental prophylaxis can interfere with bonding.
Figure 2; Crushing the provisionals with a hemostat to break them and facilitate removal.
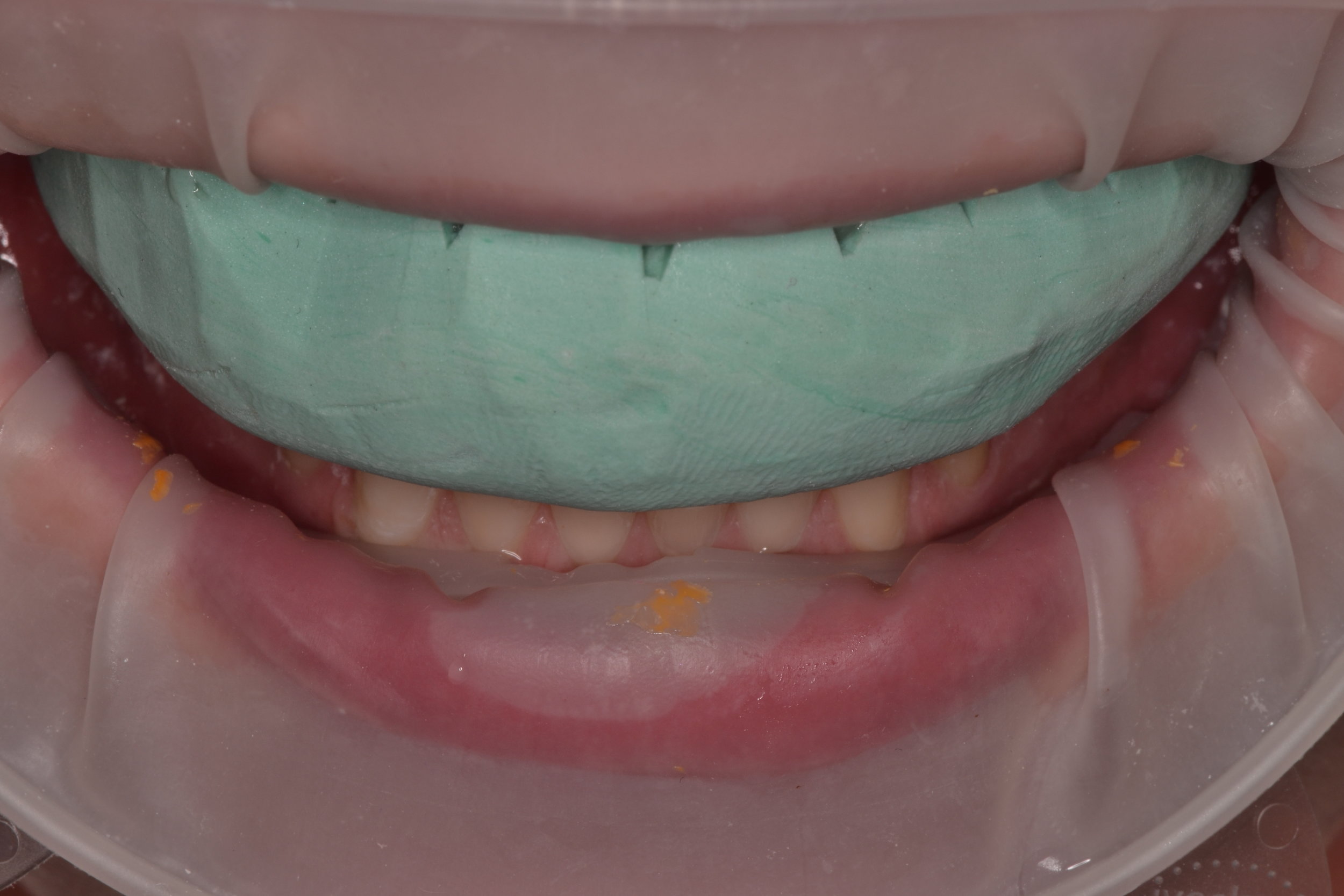
Isolation of the operative field is an essential component of performing adhesive dentistry. Rubber dam isolation is most likely considered ideal for achieving maximum isolation. For this case, an OptraGate (Ivoclar Vivadent) was used to isolate the operative field and provide retraction of soft tissues (figure 4).
Figure 4; Isolated field with retraction using an OptraGate (Ivoclar Vivadent).
Glycerin based try-in pastes are consistent in shade with the final resin cement.
Composite resin cements are consistent in shade with the glycerin based try-in pastes.
After the ceramics have been evaluated and verified for fit and composition on a stone model, individual ceramics are placed intra-orally to confirm marginal fit using visual evaluation and tactile inspection with a dental explorer (figure 5a, 5b). After the marginal adaptation and fit of each restoration is confirmed to be satisfactory, all restorations are placed onto the respective preparations with a water soluble glycerin based try-in paste (Variolink Esthetic, Ivoclar Vivadent) to evaluate interproximal contacts and the esthetic presentation of the adjacent grouping in situ (figure 5c, 5d, 5e, 5f, 5g). The advantage to the try-in pastes is two-fold. First, the paste will retain the restorations well enough for the patient to evaluate the shade and shape of the teeth, and the composition of the new smile. The patient should examine the ceramics in different light sources to ensure the effects of metamerism will not dramatically or adversely influence the shade presentation of the restorations. Second, the try-in paste will offer a replica of the final cement shade and any influence it may impart of the optics of the final restorations, namely the quality of color relating to value. In this case, the operator has three choices of try-in cements: “neutral,” which is desirable as it will impart no change on the presentation of the ceramics; “warm,” to lower the value if the restorations appear to bright; and “light,” to increase the value of the restorations if they appear to dull. The final resin cement should match the try-in paste that was confirmed during the trial arrangement. The try-in pastes are water soluble, and will rinse away will no effect on the final bond strength.
Figure 5g; Adjacent grouping of all ceramics placed in situ.
After all aspects of a cosmetic try-in are completed, and all elements of the try-in are satisfactory to the provider and patient, the steps for adhesive bonding insertion can commence.
The ceramic preparation should start at the laboratory. Ceramic materials must be etched with a hydrofluoric acid if they are to be adhesively retained. For this case, the lithium disilicate material that was chosen (eMax, Ivoclar Vivadent) was etched for 20 seconds with 5% hydrofluoric acid before being thoroughly rinsed and dried, per the manufacturer’s instructions. The parameters for the strength of HF acid and duration of contact with the ceramic vary depending on material, but the effect is the same: the acid dissolves glassy components within the crystalline matrix to create micromechanical retention via tunnels and grooves necessary for adhesive bonding. In a similar way to etched enamel, the surface of the ceramic should subsequently appear slightly frosty but clean, with no precipitate residue or cracks (figure 6a, b). After the ceramics are tried-in intra-orally, they are considered contaminated and must be cleaned prior to further preparation and delivery to ensure a high bond strength. Although reapplying 5% HF acid will sufficiently clean the intaglio surface of the restoration, HF acid is extremely caustic and has special handling considerations. Furthermore, over-etching the ceramic can create salt precipitates that interfere with bonding. Over-etching can also weaken the structural integrity of the ceramic. An alternative to re-etching with HF acid is to use a metal-oxide based cleaner with a high affinity for the phosphate chain groups that contaminate the surface to be bonded and interfere with adhesion. For this case, IvoClean (Ivoclar Vivadent) was used to remove phosphate chain groups and clean the restorations by coating the intaglio surface of each restoration for 20 seconds before being rinsed thoroughly with water and dried with an air-only syringe (figure 6c). In the case that an operator does not have these specialty items available, 37% phosphoric acid etchant can be used to coat the intaglio surface of the restoration for 60 seconds before it is rinsed and placed in water and an ultrasonic bath for five minutes. To improve bond strengths and bond durability over time, a silane coupler is applied to the clean ceramic restorations (figure 6d). By applying a silane methacrylate to the ceramic material, a chemical reaction occurs that creates a methacrylate silicate compound capable of cross-linking the silica content in the ceramic restorations with the methacrylate content in the resin cement. Multiple coats may need to be applied, and the chemical reaction will take at least 90 seconds. At this point, the ceramic restorations are fully prepared for insertion with an adhesive bonding technique, and are organized according to tooth number to avoid confusion during the procedure.
After the ceramics are adequately cleaned and prepared, the tooth structure must be prepared to receive the restorations in kind. Adequate isolation of the surgical field is required. In this case, an Optragate was used, but a solid argument can be made that a rubber dam would be the standard of care for proper isolation to employ and adhesive bonding technique. Selection of materials is paramount here, as there are a number of adhesives and resin cements on the market for the application of bonding indirect restorations to natural tooth structure. Multiple generations of adhesives and multiple iterations of resin cements have the potential to make adhesive dentistry confusing (figure 7a, 7b). When bonding to natural tooth structure, the core principles remain the same. Dentin must be etched adequately using an acid etchant. Enamel must be etched adeuately using an acid etchant.. A hydrophilic monomer (primer) must be used to infiltrate partially collagenous dentinal tubules for an appropriate amount of time. A hydrophobic monomer (adhesive) must be used to complete the formation of a hybrid layer that will link tooth structure to the methacrylate groups in composite resin cements. Moisture control and the absence of contaminants is paramount. Specific instructions and use indications will differ between the various adhesive systems and cements. It is the responsibility of the provider to use adhesive bonding systems that are compatible with the resin cement of choice.
Figure 7a
Figure 7b
The teeth are reinspected for debris or residual material and carefully polished again with oil-free flour of pumice paste.
The tooth surfaces to be bonded are etched adequately using a 37% phosphoric acid etch. If using a total etch system, the duration of etching is 25 seconds. Even in cases where an All-in-One or Universal adhesive system is utilized, etching the enamel separately is wise to ensure adequate etch. The tooth structure is rinsed for 20 seconds and then dried thoroughly using an air-only syringe. In this case, a universal adhesive (Adhese Universal Viva Pen, Ivoclar Vivadent) was applied to each tooth for 20 seconds each. The solvent was gently evaporated using an air-only syringe before being light cured for 10 seconds on each tooth. The adhesive does not necessarily need to be cured prior to insertion, but complete polymerization of the bond before insertion with a light cured resin cement will yield a higher final bond strength. Although a dual-cure cement with a compatible adhesive can be used to insert veneers, working time will become a concern with this choice, as the chemical cure of the material will commence and complete within a pre-determined amount of time.
Dr. Ryan J. Yakowicz, DDS, FAGD
Dr. Yakowicz practices in the Greater Madison Area of South Central Wisconsin. Having completed over 800 hours of continuing education, his special interests include functionally cosmetic full mouth rehabilitation, TMD and oral-facial pain, and surgical implant placement and prosthetic restoration.
Dr. Yakowicz is currently the president of the Madison Dental Progress Forum Study Club and the Wisconsin Institute for Advanced Dental Education. He is a Fellow of the Academy of General Dentistry, and a member of the American Academy of Cosmetic Dentistry, and the American Academy of Fixed Prosthodontics. Additionally, Dr. Yakowicz participates in research studies for the National Provider-Based Research Network and is an Ambassador to the National Health Service Corps.
Phasing Complex Treatment for Adolescent Patients with Orthodontic Needs
Patients presenting to to the dental office with widespread enamel defects or congenital enamel hypoplasia can present unique challenges for an operator charged with restoring the compromised teeth to proper form, function, and esthetics. These challenges are exacerbated when the patient is young or adolescent, as transitions through the mixed dentition phase and long-term appositional downward and forward growth of the maxillo-mandibular complex must often be considered. Perhaps one of the most demanding cases to address is a patient who presents with multiple criteria listed above and is in need of orthodontic treatment (figure 1a, 1b, 1c). Addressing compromised hard tissue is paramount in treating these cases, as establishing oral health will provide the basis for numerous future treatment modalities. Moreover, poor enamel quality can compromise the ability of the orthodontic provider to bond brackets when clear aligners are insufficient to address orthognathic discrepancies.
Figure 1a; A panoramic radiograph of the patient
Figure 1b; A cephalometric radiograph of the patient
Figure 1c; A retracted (1:3 magnification) view of the patient’s dentition pre-treatment
The following patient (a 17 year old male) presented with chief complaints related to his bite and the appearance of his teeth. The patient and his parent were both aware of the poor enamel quality, since older siblings have experienced the same condition. Upon initial exam, the following dental problem list was developed:
® Poor enamel quality relating to poor oral health and high caries risk
® Poor enamel quality for bonding orthodontic brackets
® Altered passive eruption
® Abnormal tooth morphology
® Dental caries, attrition, and fracture of tooth structure
® Retained primary teeth O and P with no succedaneous teeth
® Conjoined supernumerary tooth associated with the upper left second bicuspid
® Skeletal inequity affecting facial profile and causing occlusal discrepancy
® Fair oral hygiene and gingival inflammation
® Impacted third molars (#1,16,17) and upper right second molar (#2)
® Dental esthetics
(figure 2a, 2b, 2c)
Figure 2a; A retracted right lateral view (1:3 magnification).
Figure 2b; A view of the maxillary anterior teeth (1:1 magnification).
Figure 2c; An occlusal view (1:3 magnification). Note the conjoined supernumerary tooth on the mesial aspect of the upper left second bicuspid.
The patient was referred to the orthodontist for further evaluation, and the following orthodontic findings were reported:
® Class II Malocclusion
® Poor spacing and tooth size discrepancy
® Severe overjet with deep, impinging overbite
® No TMJ problems found
® Centric Relation appears to be equal to Centric Occlusion
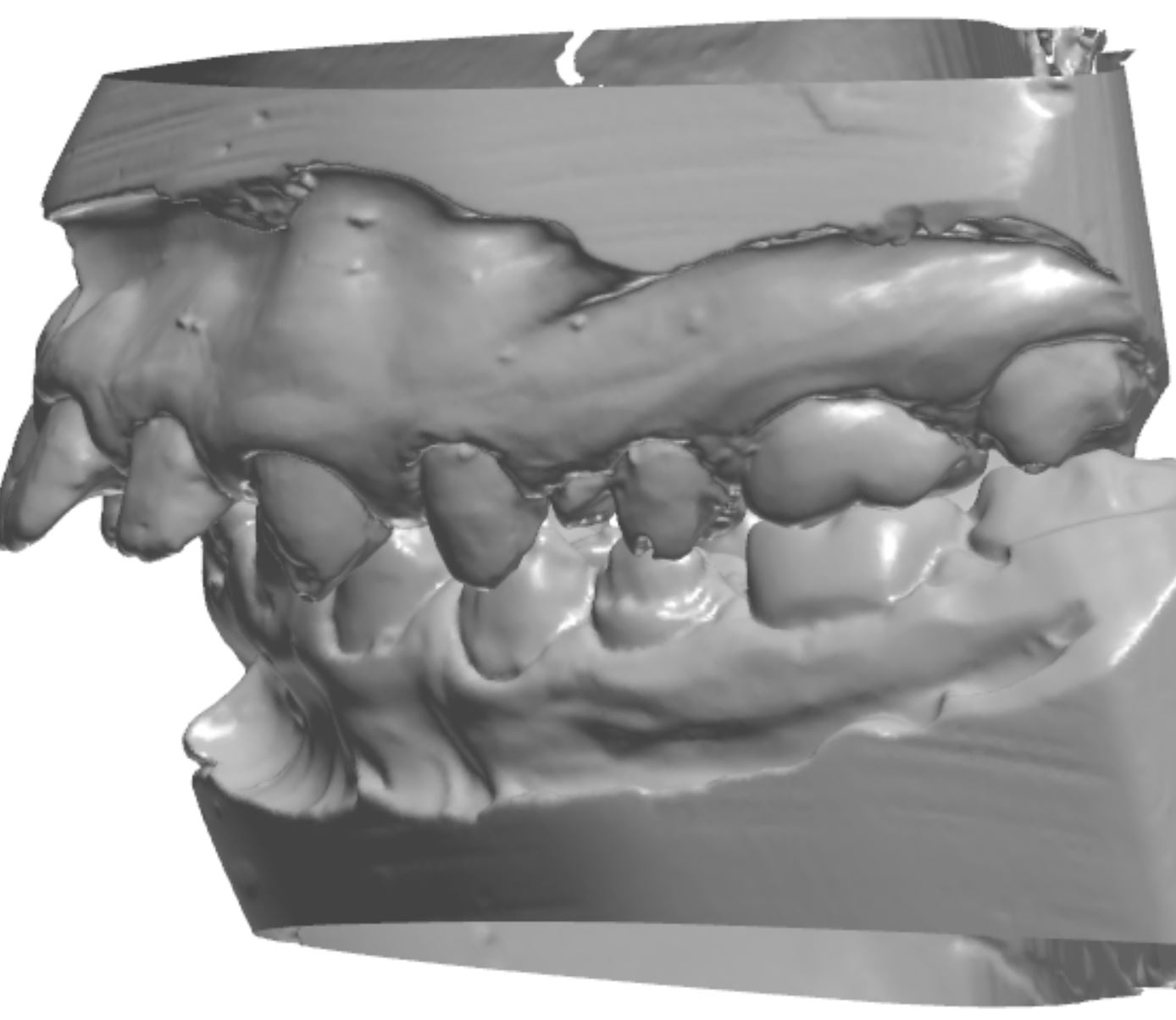
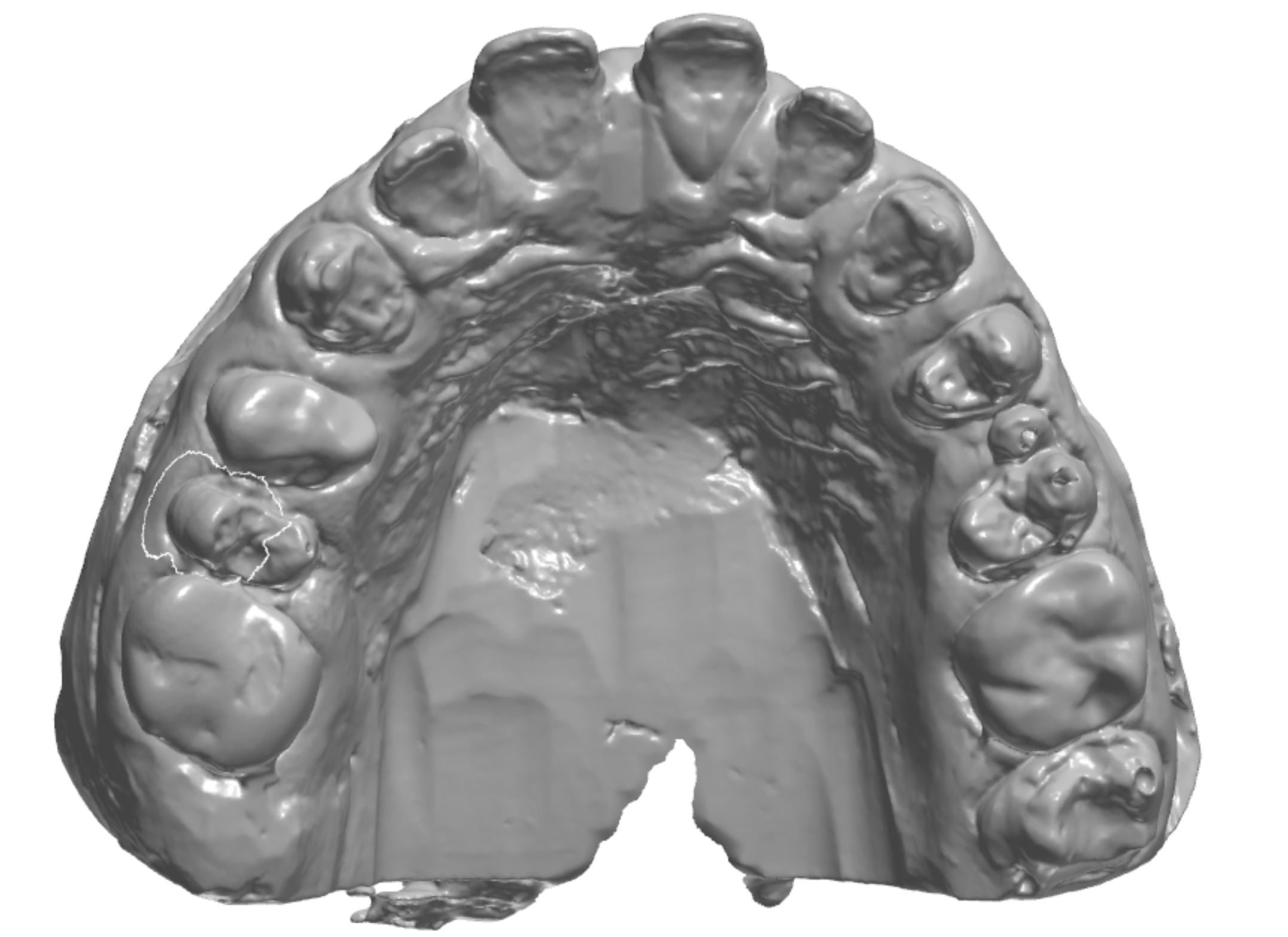
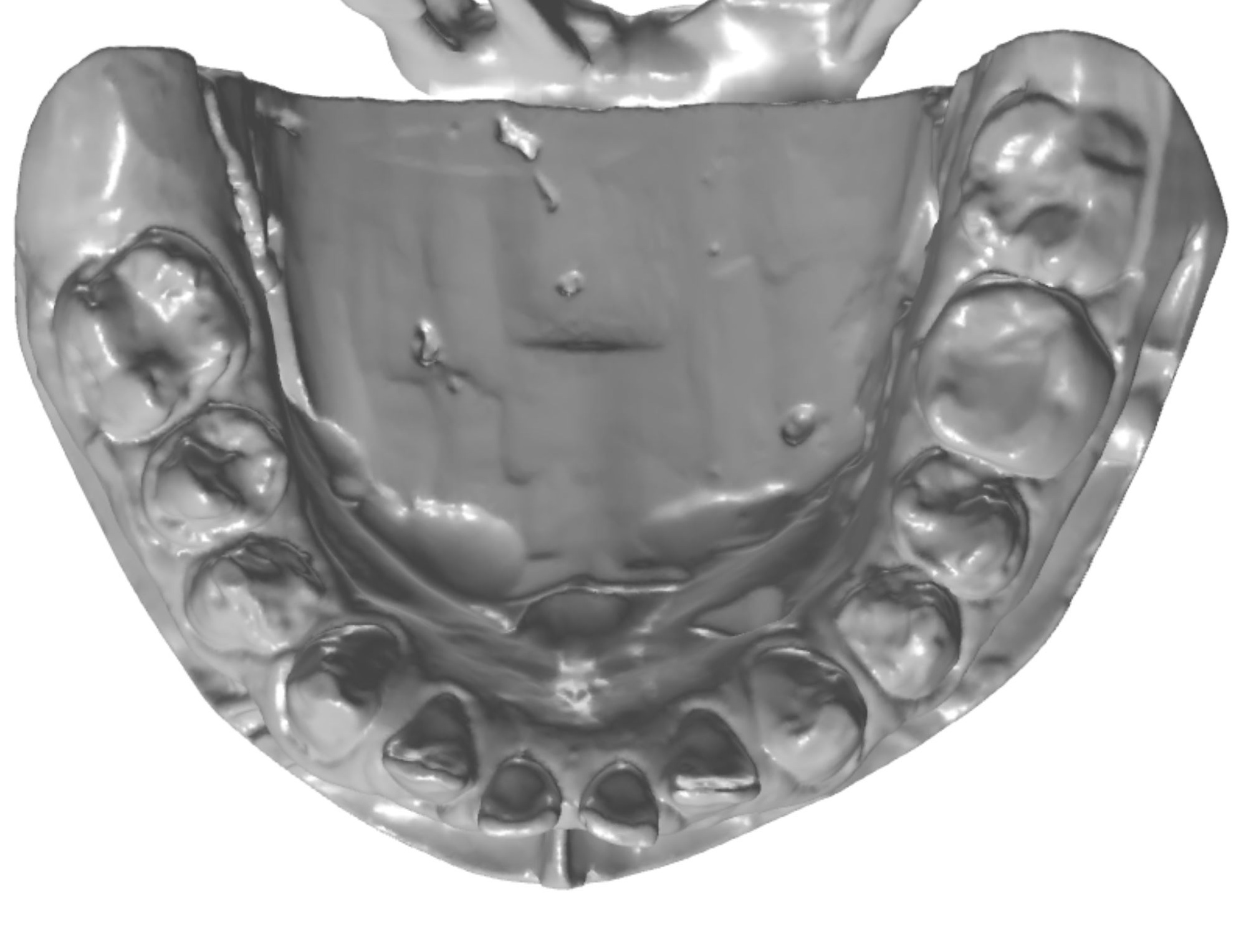
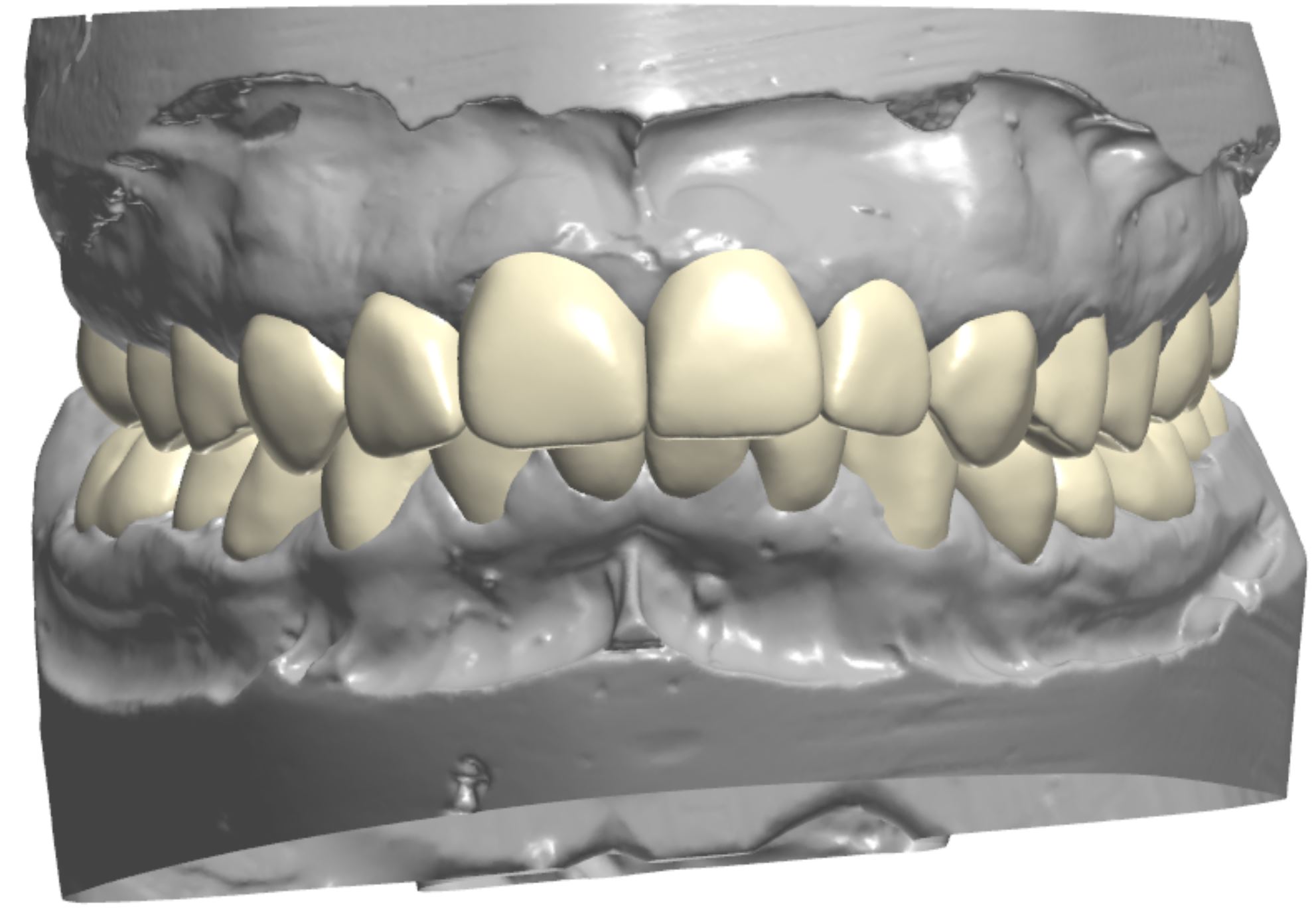
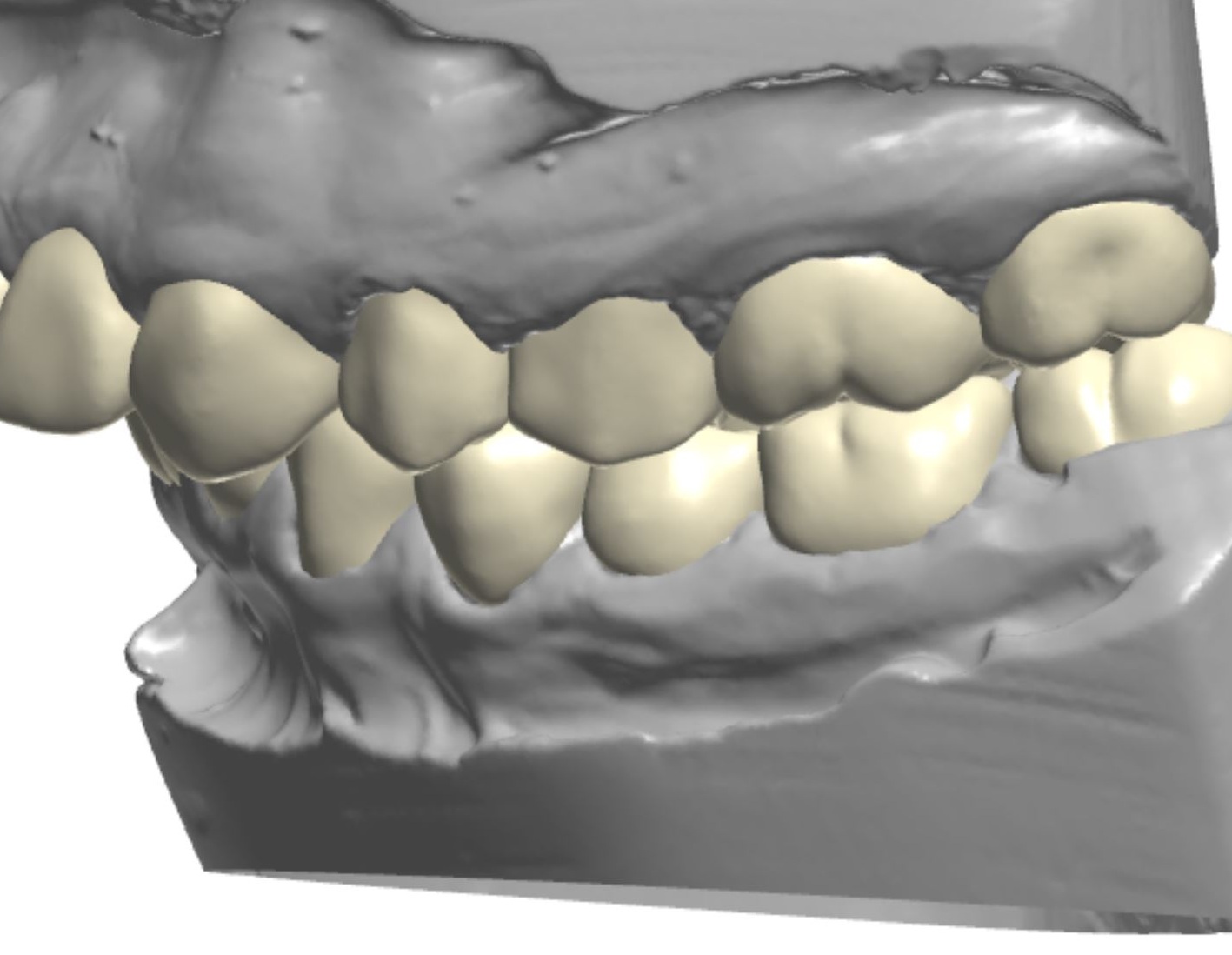
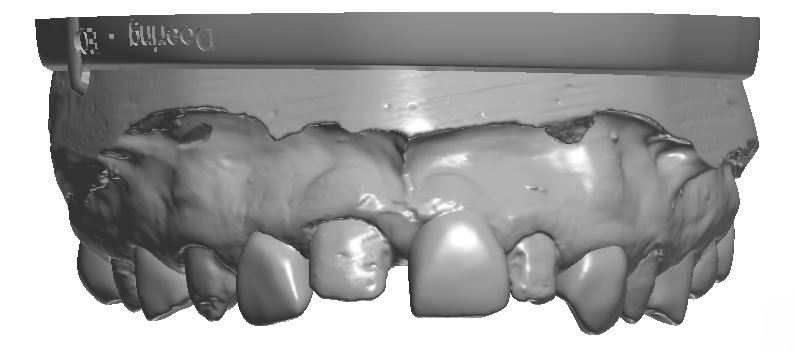
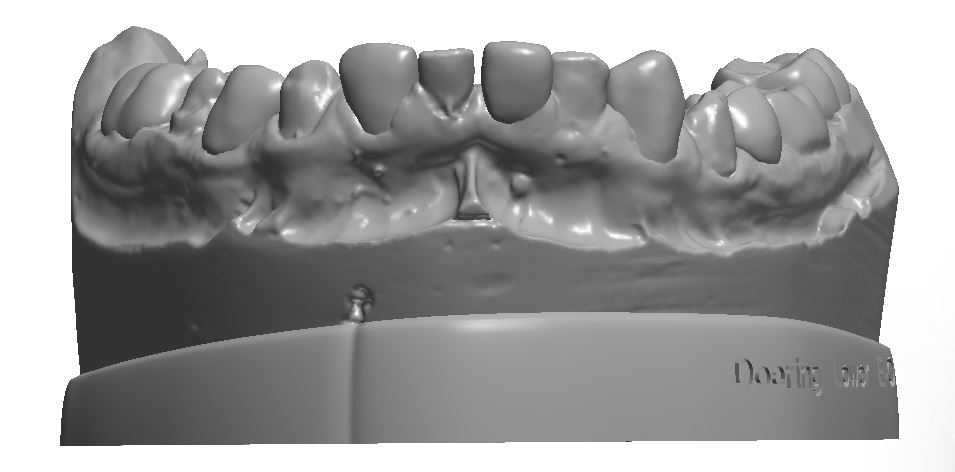
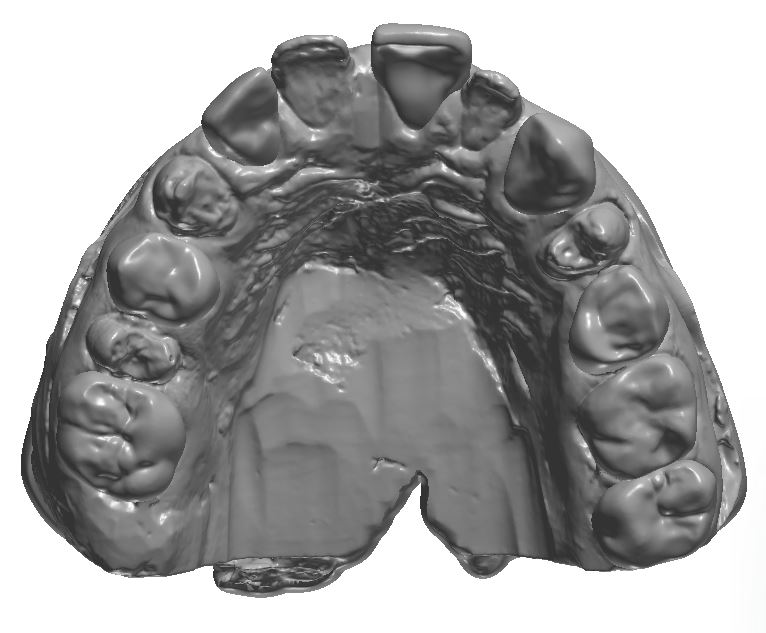
An orthodontic treatment plan was developed. Comprehensive orthodontics was recommended, with a focus on utilizing elastics and Forsus appliances to correct the Class II occlusion. Surgical mandibular advancement would be considered if non-surgical modalities proved to be insufficient in correcting the Class II occlusion. Initially, bite blocks were treatment planned to open the deep bite, but it was decided that an increase in Vertical Dimension of Occlusion (VDO) could be accomplished within the context of the restorative plan. Impressions were taken and casts were made and digitized (figure 3a). Case planning was done in combination with the restorative doctor, the orthodontist, and the digital dental laboratory technician by utilizing 3Shape Software and Computer Aided Design (CAD) (figure 3b).
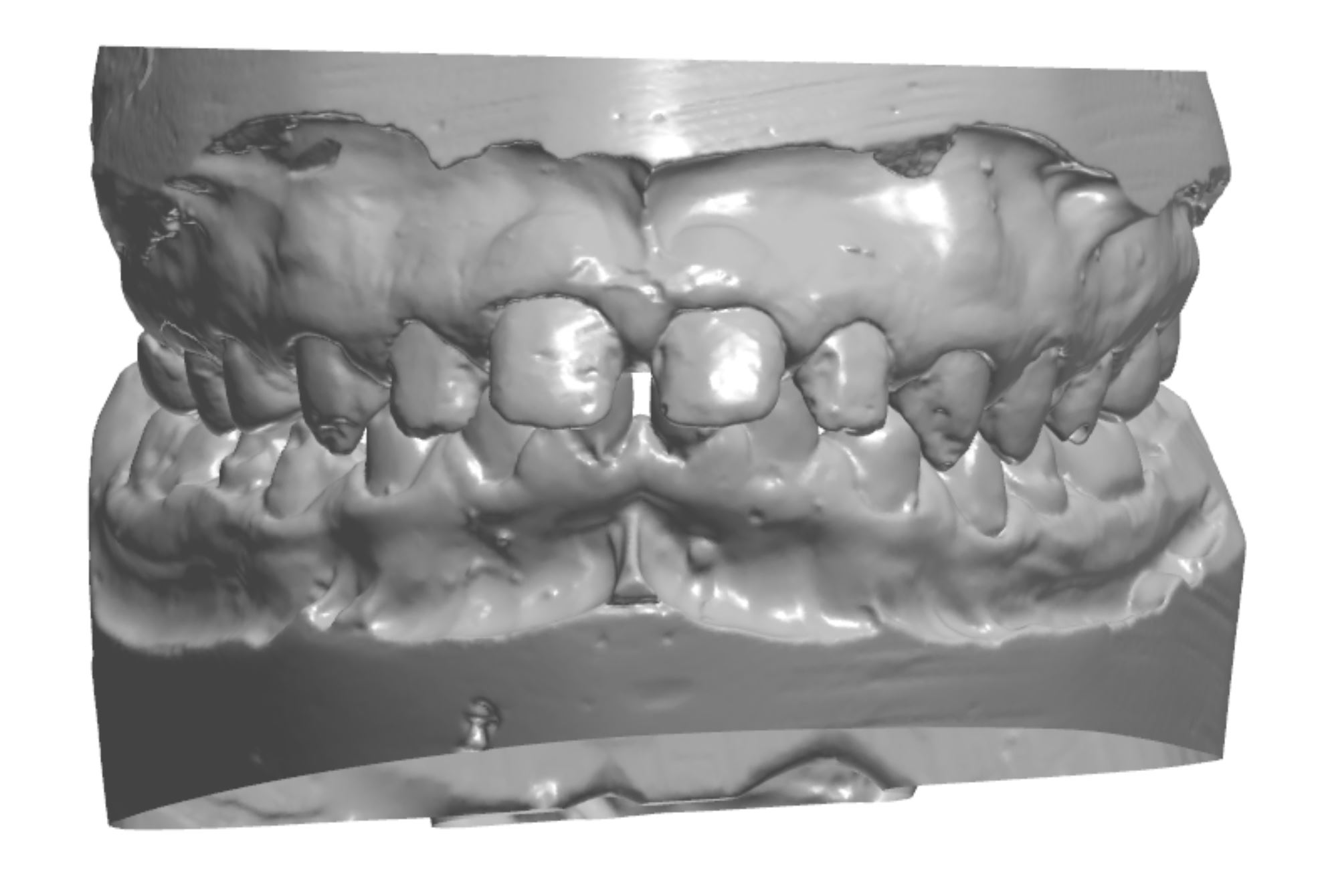
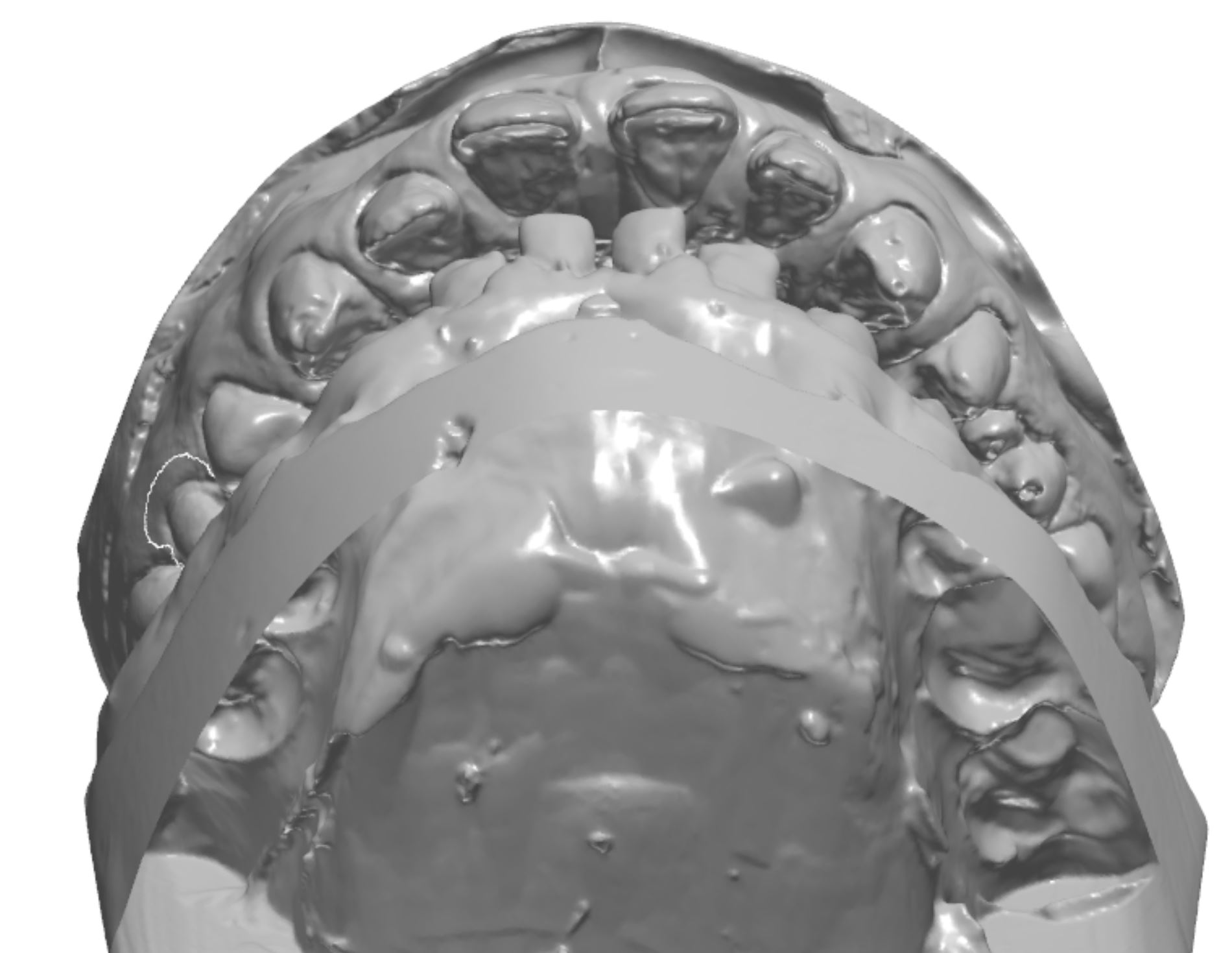
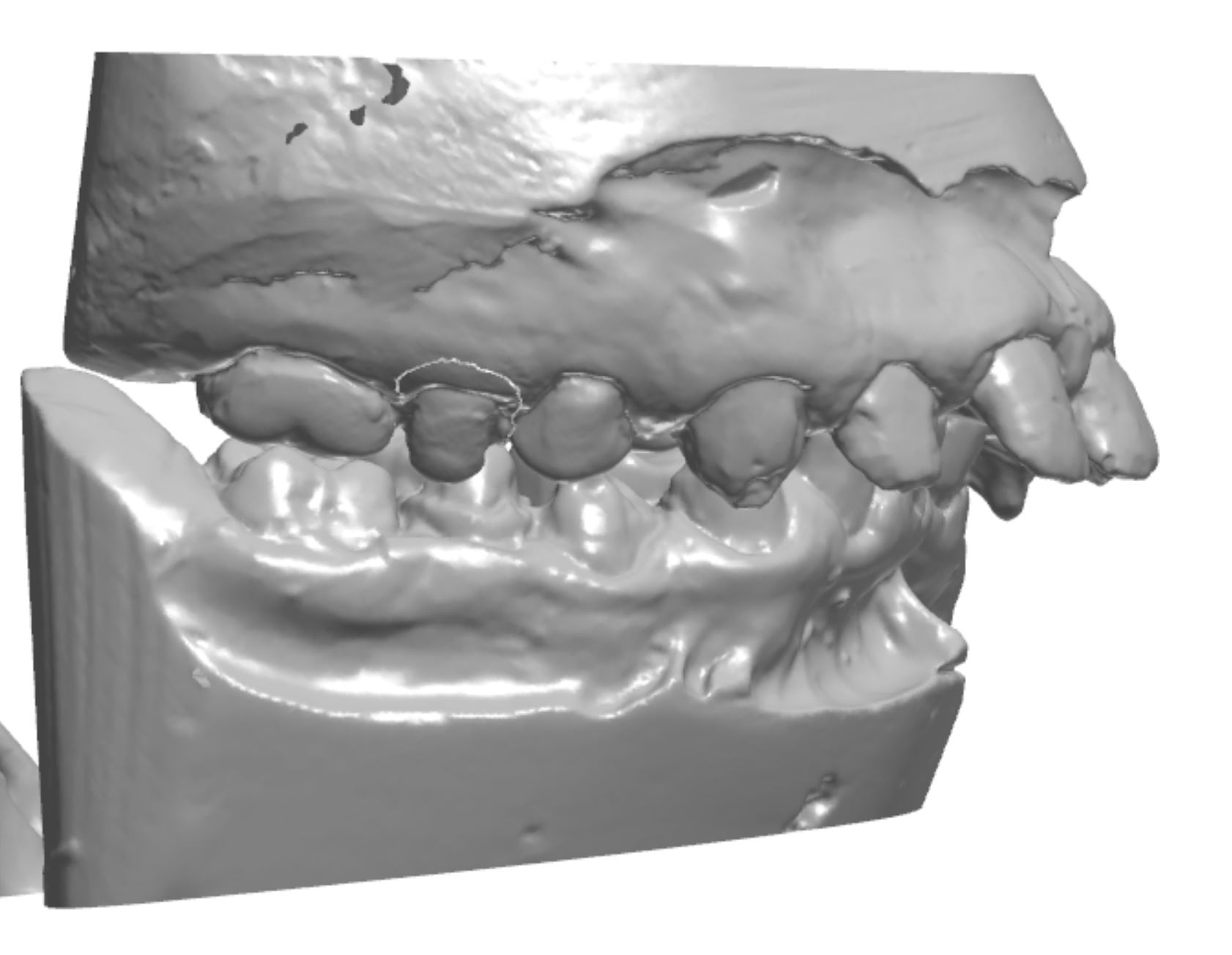
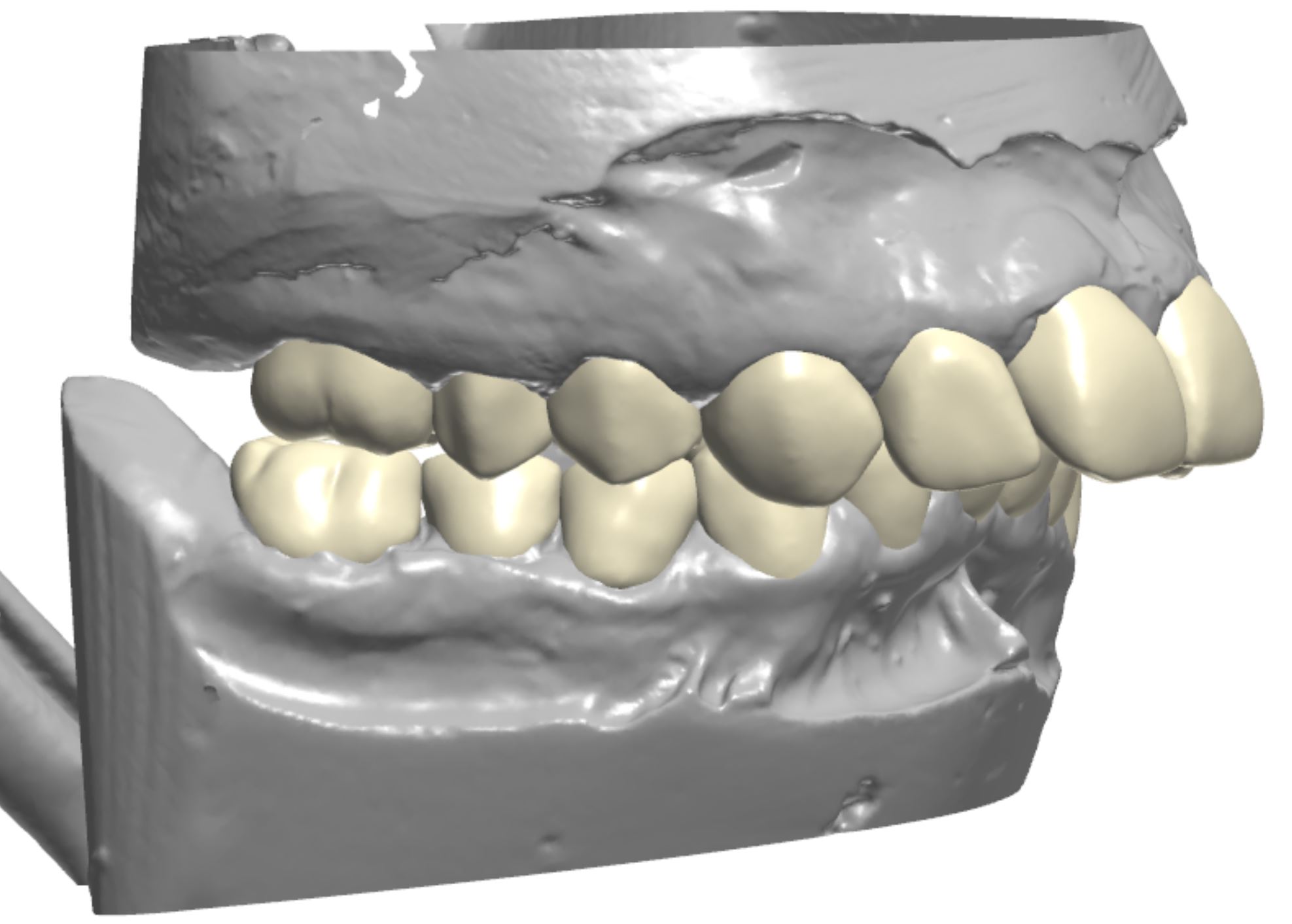
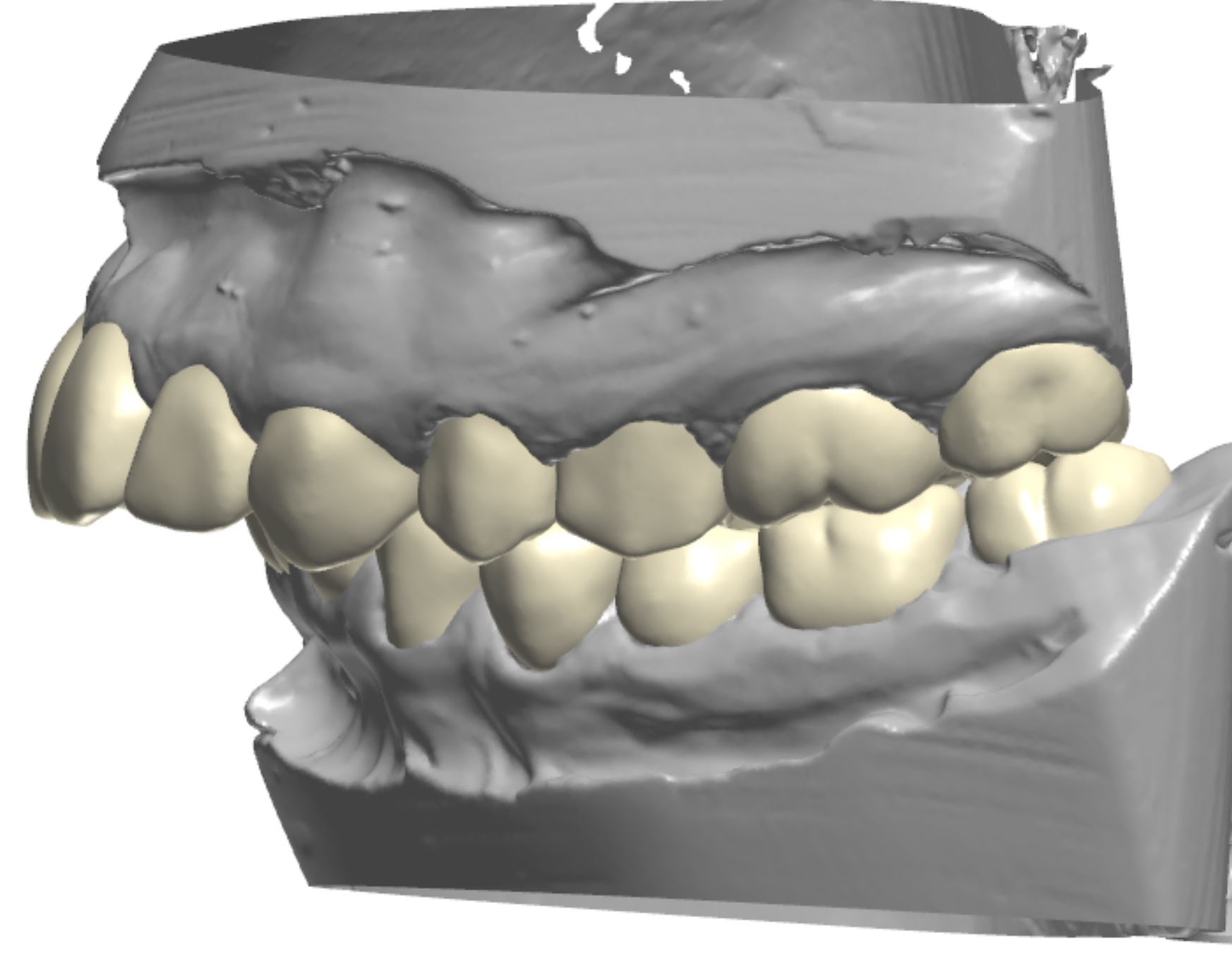
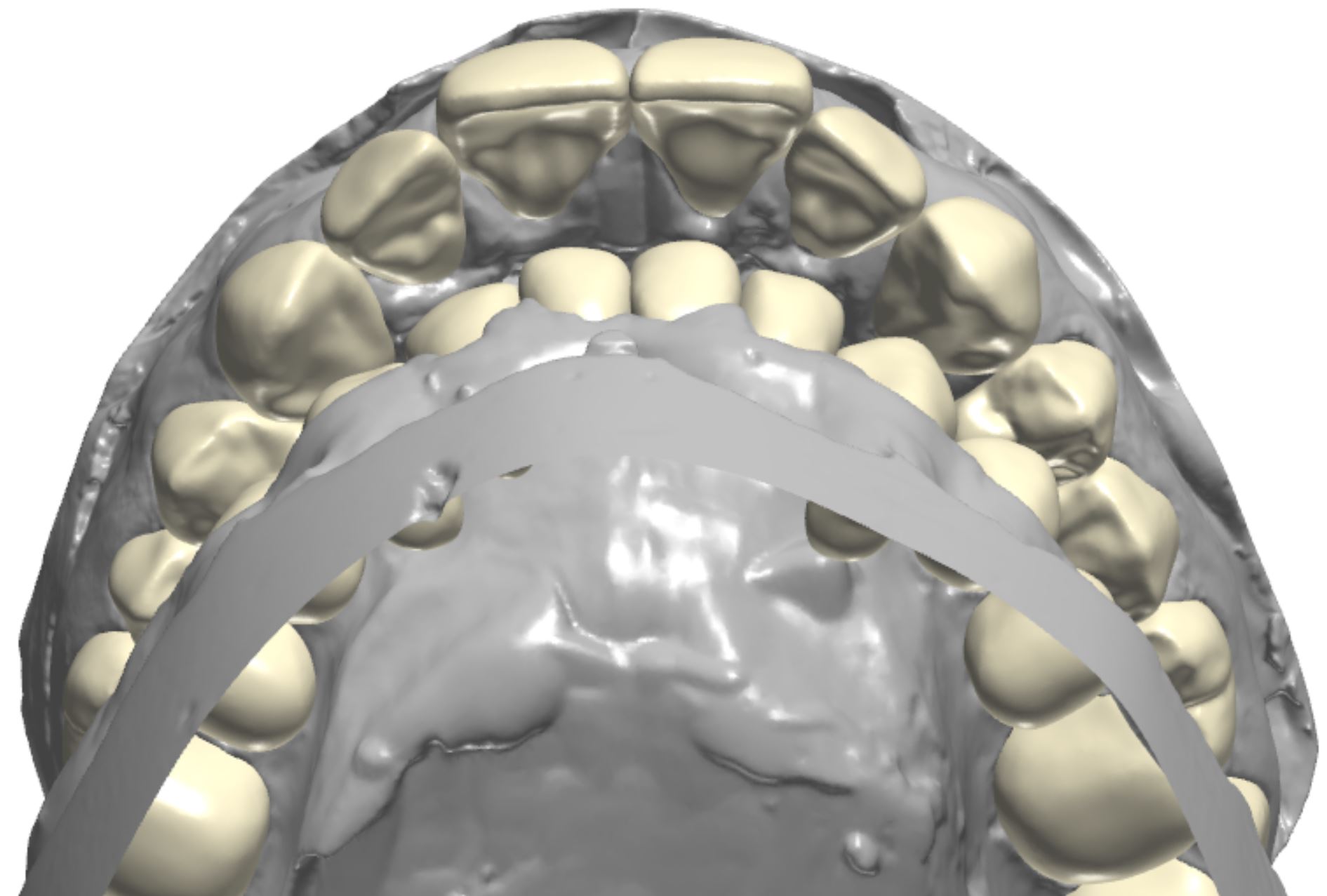
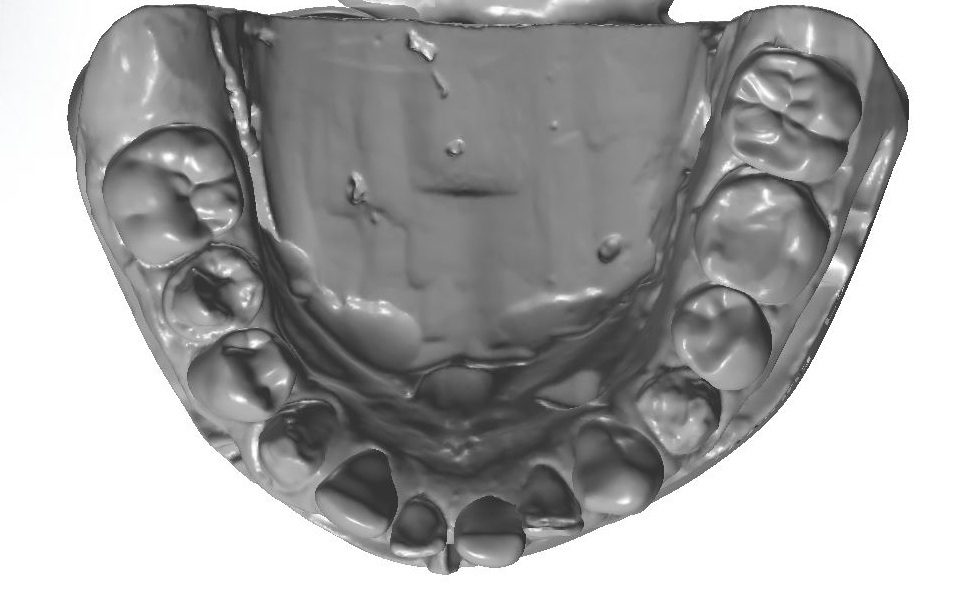
Figure 3a; Digitized pre-operative models.
Figure 3b; CAD / CAM design of the case.
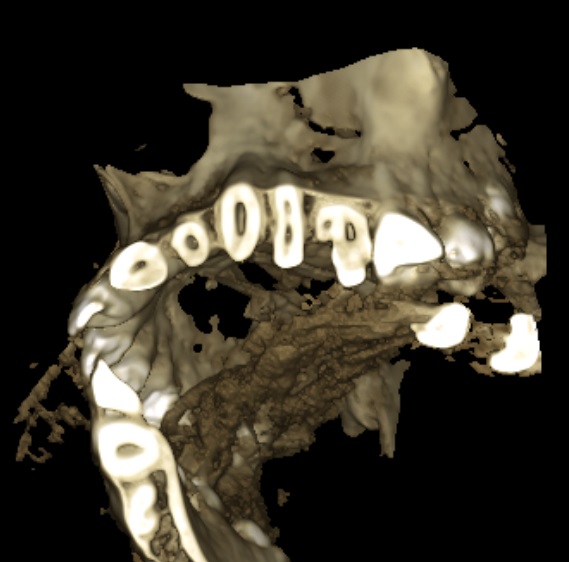
The main goals of the restorative plan were numerous and varied. Establishing oral health by removing compromised hard tissue was foundational to the success of the treatment plan. Restoring the teeth to proper form, function, and esthetics after the surgical removal of affected and infected hard tissue was considered essential to successful treatment. The restorative plan included not only esthetic correction within the limitations of the existing orthognathic condition, but also an increase in VDO to accommodate orthodontic movement of the anterior segments to correct the deep bite. The teeth needed to be restored individually to give the orthodontic provider control over root and tooth movement. Additionally, the teeth would need to be restored with a material suitable for accommodating adhesive bonding of orthodontic brackets. A final consideration in the initial restorative therapy was to provide the patient with semi-permanent restorations, as the changes to occur through orthodontic treatment and continued appositional growth would undoubtedly alter the location and presentation of the teeth within the maxillo-facial complex. Composite was selected as the most suitable restorative material to achieve the initial treatment goals. The patient was made aware that ideally, the composite crowns would be replaced sequentially with definitive dental ceramics after a proper orthodontic end point was achieved and growth was complete. Additionally, gingival plastic surgery was indicated to address the altered passive eruption, as 5-7 mm of soft tissue was present between the alveolar crest and gingival margin of multiple teeth. For initial therapy, gingivectomies with internal beveling and trans-sulcular crown lengthening would be performed to increase tooth length and maintain biological width (figure 4). Primary teeth O and P were incorporated into the restorative plan. It was decided these teeth would be retained as long as possible before extraction and definitive replacement with implants or a fixed partial denture. Initially, endodontics and removal of the supernumerary tooth conjoined to the mesial of tooth #13 was considered. After CBCT evaluation of pulp horn location, it was determined that the conjoined teeth would be treated as a single tooth, and preparation design would include the supernumerary tooth, despite a small esthetic compromise due to excessive mesial-distal width (figure 5a-b).
Figure 4; Representation of the dentogingival complex (biologic width).
Figure 5a; CBCT evaluation of tooth #13 and conjoined supernumerary tooth, along with the proposed restoration design.
Figure 5b; The modified preparation of conjoined supernumerary tooth
It was decided that the restorative plan could be used to increase the VDO to facilitate orthodontic movement of the anterior segments by creating space. Although it is arguable that this should be the primary reason for an increase in VDO, it is important to consider that bite blocks would have been implemented to create a vertical increase anyway. Additionally, it was apparent that tooth structure had been lost due to caries, fracture, or attrition in the posterior, suggesting a collapse in verticality had occured, and that replacing the lost vertical dimension should be part of restoring the posterior teeth. Caution should be implemented in increasing the VDO of patients with Class II occlusion and deep bite. As the vertical dimension (overbite) is increased, so too is horizontal dimension (overjet). This can cause problems related to speech and mastication (especially incising food) if the increase is too great. For this patient, who initially presented with a severe overbite and is committed to undergoing orthodontic treatment to better relate the anterior segments, the potential for temporary negative effects was a tolerable risk to facilitate the final outcome. As previously stated, the VDO was increased largely to give the orthodontist room to re-position anterior segments of upper and lower teeth, thereby providing the operator and lab technician with only a broad target range of how much vertical space to create. General guidelines related to increasing VDO were followed, and a 4 mm increase in VDO was agreed upon by the general dentist and orthodontist.
To address the collapsed dentition and skeletal deep bite, the maxillary central incisors and maxillary canines provided key information for planning the case. Commonly, the central incisors can help discern the amount of vertical increase needed. As a guideline, a measurement taken from the Cemento Enamel Junction (CEJ) of the maxillary central incisor to the CEJ of the lower central incisor should be 16 - 18 mm in a Class I patient and 14-16 mm in a Class II patient. These measurements can provide guidelines (not justification) for the necessity and amount of vertical increase; if the CEJ - CEJ measurements are collapsed (less than the average values) an increase in VDO may be necessary (in a standard patient). The dimension of the patient’s central incisors was deficient, especially in length, and diastemas were present. The CEJ-CEJ measurement was only 11 mm (figure 6). Increasing incisal length was done minimally and judiciously to create symmetry, as the position of the central incisors and incisal edge in the patient’s face was appropriate. Tooth length gain could however be accomplished in an apical direction by performing gingivectomy with internal beveling. When sounding bone, it was discovered that the alveolar crest was located 4 - 6 mm from the gingival margin in the anterior segment, confirming that the actual CEJ of the maxillary central incisors is positioned more apically than the gingival margin would suggest. By relieving 3 mm of soft tissue and severing the connective tissue attachment, a 3 mm gain in tooth length could be achieved while still providing 3 mm for biologic width. In areas where 3 mm of space to accomodate biologic width was not available, a chisel was used to remove small amounts of the crestal bone through the sulcus (figure 7a-e). A new measurement from CEJ-CEJ would then be 14mm, which is more normative for a Class II patient. Only the canines were treated with plastic surgery at the time of initial treatment. Although evaluation of the dento-gingival complex relating to the central and lateral incisors was essential for treatment planning, it was decided surgery would be done after re-evaluation when a stable orthodontic endpoint was reached and growth was complete.
Figure 7a-e; a) Periodontal probe reading of the sulcular depth is 3 mm. b) When sounding bone, the periodontal probe reading approaches 6 mm. c) Gingivectomy to relieve excess tissue and contour gingival shroud (note the amount of enamel apical to the initial gingival margin posititon). d) Internal bevel to sever the connective tissue attachment. e) a bone chisel with a laser etched 3 mm marking to ensure adequate space for biologc width between the crestal bone and the new gingival margin position.
As detailed by Dr. Carl Misch, the canine position is a key indicator for planning tooth position relative to the maxilo-facial complex. Although some apical gain could be created by performing gingivectomy on the canines, it was clear that orthodontics would be required to continue apical movement to position the teeth (especially the canines) in the proper location. Although 3 mm worth of gingivectomy could help with the canine tooth length, apical gain alone would not be adequate to position the teeth correctly in the maxillo-facial complex. The acceptable range for canine exposure in relation to the maxillary lip line varies, but Misch found that the range of canine display in a lip at rest position varies far less than that of central incisors. Our goal for the patient was to have 0-1 mm of the canines visible in a lip at rest position. Gingivetomy with internal bevel and trans-sulcular bone removal was to be performed, but it was determined that the canine would still need to move apically 3 mm to be in the proper location in the face. Because the initial restorative phase would be interim in nature, the VDO change could be adjusted as necessary; either to accommodate orthodontic movement or to relieve possible TMD symptoms due to the patient being unable to accommodate the new VDO.
Figure 6; CEJ-CEJ measurement (11 mm) and maxillary right central incisor measurement (8 mm long x 8 mm wide).
Overall, the case was designed as a full mouth rehabilitation. The design included considerations related to tooth proportion, gingival zenith location, increased vertical dimension, esthetic correction, and stable occlusion. The plan was representative of initial therapy with the intention of being revisited after completion of orthodontic treatment.
Transfer of the plan to the patient’s dentition was completed using deliverables from the dental laboratory and composite resin. In the Computer Aided Design / Computer Aided Manufacturing (CAD / CAM) software, the complete design of the corrected maxillary and mandibular arches was printed using a 3D printer. Then, the initial design was altered so that only every-other tooth was corrected, while every-other tooth remained in its pre-operative state (figure 8). A set of models representing a correction of every-other tooth for each arch was also printed. Clear matirces were made on each set of models. Clinically, the patient was anesthetized, and soft tissue corrections were made using a 15C Scalpel and bone chisel. Next, every-other tooth was treated by removing unhealthy hard tissue before being prepared for the composite restoration. Retraction cord was placed in the gingival sulcus of the prepared teeth. The unprepared teeth adjacent to the prepared teeth were protected with strips of sterilized polytetrafluoroethylene (PTFE) tape to prevent unintentional adhesive bonding. A 37% phosphoric acid etch was used in a total etch technique, desensitizer (MicroPrime G, Danville) was applied to the prepared tooth structure and adhesive (Prime&Bond Elect Universal Dental Adhesive; Denstply Sirona) was applied for 20 seconds and light cured for 10 seconds. The clear matrix was fit over the unprepared teeth and shade A2 flowable composite (Herculite Ultra-flow Nano-hybrid; Kerr) was injected through a porthole created in the matrix prior to placement (figure 9a-d). The composite was cured through the matrix for 20 seconds on each surface; the excess material was trimmed and the restorations were contoured before the next set of teeth were prepared (figure 10a-b). This process was repeated for the remaining teeth. The occlusion was adjusted as necessary and the final composition was then polished. The patient was re-appointed for a 3-week re-evaluation to ensure the increase in vertical dimension was not problematic, and that stomatognathic functions such as eating, swallowing, and speaking were not compromised.
Figure 8; The “every-other” model in CAD / CAM software.
Figure 9a-d;
Figure 10a;
Figure 10b;
Ultimately, each tooth was restored individually to enable individual orthodontic root and tooth movement while providing a bondable substrate for orthodontic brackets. Although provisional, the restorations offered the patient immediate improvements in oral health, and in the form, function, and esthetics of his teeth. Furthermore, because the restorations are not considered definitive, the prototype is dynamic and able to be altered during continued restorative and orthodontic treatment; unlike dental ceramics, composite can be easily removed from or added to. Furthermore, the living prototype will provide valuable information before the dentition is to be definitively restored. Although cases like these require intensive planning pre-clinically and many chair hours clinically, the initial improvements are extremely rewarding. Given proper treatment planning and coordination between the operator, orthodontist, and lab, cases like this can be extremely fun to execute!
Dr. Ryan J. Yakowicz, DDS, FAGD
Dr. Yakowicz practices in the Greater Madison Area of South Central Wisconsin. Having completed over 775 hours of continuing education, his special interests include functionally cosmetic full mouth rehabilitation, TMD and oral-facial pain, and surgical implant placement and prosthetic restoration.
Dr. Yakowicz is currently the president of the Madison Dental Progress Forum Study Club and the Wisconsin Institute for Advanced Dental Education. He is a Fellow of the Academy of General Dentistry, and is a member of the American Academy of Cosmetic Dentistry, and the American Academy of Fixed Prosthodontics. Additionally, Dr. Yakowicz participates in research studies for the National Provider-Based Research Network and is an Ambassador to the National Health Service Corps.
References:
1) Spear, F (2006) Approaches to Vertical Dimension. Advanced Esthetics and Interdisciplinary Dentistry 2 (3): 2006: 2-12.
2) Kois, J, Phillips, K (1998) Occlusal Vertical Dimesnion: Alteration Concerns. Compendium 18 (12): 1998: 1169-1177.
3) Rivera-Morales WC, Mohl ND. Relationship of occlusal vertical dimension to the health of the masticatory system. J Prosthet Dent. 1991 Apr;65(4): 547-53.
4) Terry, Douglas A., Willi Geller, and Douglas A. Terry. 2013. Esthetic & restorative dentistry: material selection & technique. Chicago: Quintessence Pub. Co.
5) Misch, CE. Guidelines for maxillary incisal edge position-a pilot study: the key is the canine. J Prosthodont. 2008 Feb;17(2):130-134.
6) Terry D, Powers J, Blatz M. The Inverse Injection Layering Technique. Journal of Cosmetic Dentistry. 2018 Spring; 34 (1): 48-62.
7) Coachman, C. Emotional Digital Dentistry. Journal of Cosmetic Dentistry. 2019 Winter; 34 (4): 36-42.
8) Lyons, L, English, J. In Vitro Shear Testing of Orthodontic Bonding to Lithium Disilicate Ceramic. Journal of Cosmetic Dentistry. 2019 35 (1): 82-89.
Start to Finish Veneers: Part 2, Preparation and Provisionalization
It must be said that there are many methods for preparing teeth for cosmetic restorations such as labial veneers. The comfortability and personal preference of the operator that best suits his or her skill set and background in cosmetic restorative dentistry is not to be overlooked. What follows is simply one method to achieve pre-planned restorative goals of the operator and patient.
Figure 1; The prototype of the desired outcome transferred intra-orally.
After the prototype is verified by the patient and the dentist, the preparation phase of treatment can commence. The patient is anesthetized and an Optragate (Ivoclar Vivadent) is used for general isolation and retraction. The prototype is not removed, but rather utilized as a facial and incisal reduction guide that is based on the final objective. By leaving the prototype in place, tooth reduction can be performed relative to the restorative plan instead of being performed relative to the existing tooth surface. Different portions of different teeth may require more or less reduction to create a near-uniform space that will accommodate the thickness of the selected restorative ceramic material without unnecessarily removing hard tissue. The operator should perceive this process as an exercise in creating minimal space to achieve the restorative outcome, which is a very different perspective than removing a certain amount of tooth structure solely due to a preset preparation parameter. For this case, lithium disilicate (IPS e.Max, Ivoclar Vivadent) was selected as the restorative material for its esthetic qualities, flexural strength, and ability to be bonded using an adhesive resin cement. According to the manufacturer, veneer thickness should be between 0.3 mm and 0.7 mm depending on what portion of the tooth is being restored, what material is being used, and whether the restoration will be milled or pressed[1]. This is more or less consistent with instructive literature regarding tooth preparation for bonded ceramic veneers[2]. For this case, the goal was to create a space to accommodate ceramic restorations that would be 0.5 mm – 0.7 mm thick in the facial and interproximal areas, with slightly less space considered in the cervical-facial planes of the teeth and slightly more space considered in the middle-facial and incisal-facial planes of the teeth. The necessary space for the incisal edge would be 1.5 mm to fulfill both the functional occlusal demands of the restorations and allow the ceramic technician space to create micro-esthetics and translucency at the incisal edge of the restorations.
Figure 2; Depth cuts through the in-place mock-up.
Figure 3; 834 - 021 M diamond depth cutting bur (0.5 mm).
To achieve this, depth cuts are made through the mock-up (figure 3) using a 0.5 mm depth controlled bur (834 – 021 M, figure 3). Care is taken to advance the bur into the proximal areas, as adequate space for the indirect restoration is often not attained in this area. By leaving the prototype in place and using a bur with controlled depth, areas requiring more tooth removal to achieve the final design with ceramic veneers are indicated. Likewise, areas where space for the outcome already exists without preparation can also be identified. To ensure adequate incisal reduction, a cylindrical modified bevel bur is used (878 – 016, figure 4a). This bur can continue be used for axial reduction of tooth structure, but the important thing to consider here is depth control: Any cylindrical bur with a diameter of 1.4 or 1.6 mm can be used to indicate an incisal depth of very close to 1.5 mm (figure 4b). After initial depth cuts are made in the facial and incisal portions of the prototype (figure 4c), the extent of the preparation is marked with a sterilized pencil (figure 4d). Axial preparation is continued through the prototype until the acrylic material is removed to the level of the initial depth cut markings facially. The incisal edges are reduced to the level of initial notching with the 878 – 016 bur and the acrylic is removed before the preparation design continues with the aid of the incisal reduction guide and facial reduction guide (figure 4e). Respect should be given to the amount of enamel present for each individual patient, and as much of the preparation as possible should be located in enamel in an effort to conserve tooth structure and maximize adhesive bond strength.
Figure 4e; The completed facial reduction of the maxillary left central incisor.
Although many preparation designs for ceramic veneers have been proposed, there are some general guidelines to consider. First, a light chamfer finish-line should be utilized in the cervical and interproximal portions of the preparations. A round end taper diamond (856L) or modified beveled cylinder (878) in the 1.4 to 2.0 mm diameter range can be used to axially reduce tooth structure and create light chamfer margins. The finish line should follow the gingival contours and should be placed at or slightly (0.5 mm) below the gingival margin. In most cases, the finish line should be continuous with the lingual extent of a butt margin on the incisal edge to create a partial or total wrapping of the preparation. This design will prevent high tensile stresses associated with finish line extension down the palatal surface.[3,4] Placing the margin on areas with existing static or dynamic occlusal contacts should be avoided. Second, breaking interproximal tooth contact can create numerous advantages. By breaking contact, the finish line can be better captured in the final impression, margins of the final restorations will be less visible, and the ceramic technician will be afforded more freedom in approximating adjacent restorations and establishing appropriate tooth contacts (figure 5a). Although breaking contact is commonly done in cases where a large shade change is desired and in cases of diastema closure, it is not always necessary. If tooth contact is not broken, care should be taken to create an “elbow” underneath the contact area to hide margins that may be visible. Lastly, the preparation should be smooth (figure 5b). Taking time to polish preparations can offer the operator an opportunity to carefully inspect each preparation for sharp angles or hindrances to path of insertion of the restoration, and alter the prep as needed.
Figure 6; Interproximal caries discovered during initial tooth preparation
Of course, these guidelines are theoretical until surgical removal of tooth structure commences. Incidental findings such as decay or existing dental restorations can certainly influence preparation design for ceramic veneers. In this case, carious lesions were noted on multiple teeth during initial preparation (figure 6). Moreover, pre-existing restorative material on three of the four treated bicuspids was removed to ensure hard tissue health before proceeding with preparation design. After further discussion with the patient and laboratory, it was also decided that a conservative crown preparation on the maxillary left lateral incisor would produce a better functional and cosmetic result than an aggressive veneer preparation.
After pre-existing restorative material and caries were removed, tooth preparation was refined and finalized before an impression was made. As previously stated, the preps were polished during this process to ensure that there were no sharp line angles and no undercuts or impedances to a path of insertion. A size 0 cord was placed in the depth of the sulcus, followed by a size 1 deflection cord placed more superficial to the sulcular cord. Desensitizer (Microprime G, Danville Products) was applied to the prepared tooth structure and blotted dry before impressing. The more superficial cord was removed from the sulcus before the impression was made, and the deeper sulcular cord remained in place to act as a barrier to crevicular fluid or heme (figure 7a, 7b).
The final impression can be taken conventionally by placing a light body PVS wash material around the preparations while a tray is loaded with a heavy body or putty impression material is seated over the teeth to be impressed. Alternatively, a method where the tray is loaded with putty and a trough is made and then filled with the lighter body wash material before being seated can also be used. Clearly, an accurate impression is paramount. In large cases like this, there may be one or two small but important details that are not captured accurately in the total impression. If this occurs, making a supplemental impression that focuses on the information that needs to be captured more accurately can be made. The dental laboratory can then make a working die or margin die of one or two teeth without sacrificing the harmony of the composition during fabrication.
After an accurate impression of the preparations is made, an equally accurate impression of the opposing arch is made. An inter-occlusal record is made with the patient in an upright position. For this case in particular, each of these steps were imperative, as changes to the occlusal surfaces had been made as part of equilibration treatment.
Figure 8; Die shade tab photo (photos of ND1 and ND2 were both provided to the dental laboratory)
Prior to temporization, die shade photos were taken to communicate with the dental laboratory, as the underlying tooth structure is vital information in cases of shade improvement with ceramic veneers (figure 8). Next, the preparations were spot etched, rinsed, and dried (figure 9a,b) before primer (Optibond XTR Primer, Kerr) was painted on to the preparations and air-dried (figure 9c). A shrink-wrap technique was used to provisionalize this case. The silicone putty matrix made from the diagnostic mock-up was again loaded with a provisional material (Visalys Temp, Kettenbach Dental), placed over the prepared teeth, and allowed to auto-cure (figure 9d,e). The matrix was carefully teased off of the teeth so as not to lift the recently adapted temporary material from the prepared tooth surfaces. The notches cut into the matrix help limit the amount and severity of flash (figure 9f). Gross removal of excess material can be accomplished a scaler or similar instrument (figure 9g,h) before rotary instrumentation is used to trim the margins, contour the provisionals, and open gingival embrasures for hygiene purposes. Some burs to consider for this are the 889-010 diamond separating bur (fine) and the 863-016 diamond flame bur (super fine)(figure 9i,j respectively). Rotary discs of varying grits (FlexiDisc, Cosmedent Inc., figure 9k) were used to further contour and polish the provisional restorations. The occlusion is adjusted as necessary. Once the occlusion is verified, the esthetics are approved and the composition is polished (figure 9l,m).
Figure 9m, The finalized provisional restorations on the preparation day.
Figure 10; passing super-floss through healthy gingival embrasures post-operatively.
Patients are given hygiene instructions for the provisional phase of treatment. Since the temporary restorations are connected in the shrink-wrap technique, the patient is asked to use super-floss (or a floss threader) twice a day and is shown how to thread the floss through the opened gingival embrasures (figure 10). The patient is given a Water-Pik and is advised to use it on a relatively low setting (3) for the duration of wearing the temporary restorations. The patient is asked to brush normally, and is given Chlorhexidine Gluconate 0.12% for nightly use. Of course, other modalities such as interproximal brushes or rubber tip simulators can be recommended as the idea is to encourage the patient to maintain exceptional gingival health in an effort to create a favorable environment for an adhesive bonding technique at the time of ceramic restoration insertion.
The patient is re-appointed for evaluation 2 weeks after tooth preparation. Patient feedback about esthetics (including shade), function, and bite comfort are discussed, and necessary adjustments are made. Once the patient and dentist are satisfied, a high-quality impression of the provisional arrangement is made and sent to the lab to communicate incisal edge position and occlusal scheme. Select photographs are also taken for adjunct communication tools (figure 11a-h). In this case, neither the dentist or the patient were happy with the shade of the temporary restorations. New shade tabs of the patient’s desired outcome relative to the current restorations were taken to share with the lab. Finally, the patient is appointed for insertion of the definitive restorations.
It is clear that cases like this are demanding of a clinician’s time, skill, and artistic ability. Thorough planning and execution, as well as the flexibility and ability to change preparation design intra-operatively, are imperative to success. Overall, preparations like this can be extremely rewarding, and very fun to do.
Dr. Ryan J. Yakowicz, DDS, FAGD
Dr. Yakowicz practices in the Greater Madison Area of South Central Wisconsin. Having completed over 775 hours of continuing education, his special interests include functionally cosmetic full mouth rehabilitation, TMD and oral-facial pain, and surgical implant placement and prosthetic restoration.
Dr. Yakowicz is currently the president of the Madison Dental Progress Forum Study Club and the Wisconsin Institute for Advanced Dental Education. He is a Fellow of the Academy of General Dentistry, and a member of the American Academy of Cosmetic Dentistry, and the American Academy of Fixed Prosthodontics. Additionally, Dr. Yakowicz participates in research studies for the National Provider-Based Research Network and is an Ambassador to the National Health Service Corps.
References:
[1] IPS e.max Clinical Guide. https://www.ivoclarvivadent.com/en/p/all/products/all-ceramics/ips-emax-dentist/preparation
[2] Magne P, Besler U. Bonded Porcelain Restorations in the Anterior Dentition: A Biomimetic Approach. Chicago, IL: Quintessence, 2003: 239-246.
[3]Magne P, Douglas WH. Design optimization and evolution of bonded ceramics for the anterior dentition: a finite-element analysis. Quintessence Int. 1999 Oct;30(10):661-72.
[4]Chai, Sy Yin et al. Incisal preparation design for ceramic veneers. The Journal of the American Dental Association. 2018 Jan;149(1): 25-37.